
LEONARDO MASTROPASQUA, MD
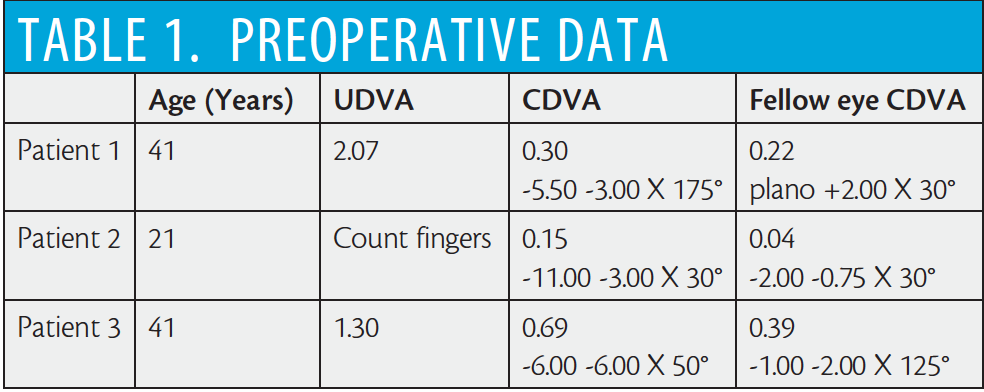
In the presence of corneal diseases in which the endothelium is preserved, such as in keratoconus, deep anterior lamellar keratoplasty (DALK) has the advantages of reduced immune rejection of the endothelium and minor loss of endothelial cell density (ECD).1 As with PKP, however, resultant anisometropia after DALK can decrease the overall success of the procedure.
AT A GLANCE
• SMILE can be considered a treatment option for myopic and/or astigmatic refractive error after DALK, in particular in patients who experience anisometropia or contact lens intolerance after the transplant surgery.
• The results of the authors’ case series showed several advantages in the application of SMILE after DALK: no symptoms of ocular discomfort or pain; no haze, graft rejection, or dry eye; reduction of tissue edema and inflammation; and no ectatic disorders of the posterior corneal surface.
In fact, high astigmatic and/or myopic refractive errors are the most frequent refractive complications after DALK. Several studies have reported that DALK can result in significantly higher myopia than PKP.2-4 High spherical refractive error after DALK in keratoconic eyes has been shown to result mainly from elongation of the posterior segment of the globe. Additionally, smaller contributions are made due to the steepness of the corneal graft5 and to the fact that grafts conform, partially, to the curvature of the recipient Descemet membrane (DM), which remains intact in the closed-system DALK procedure.2,6
Donor graft size, donor-recipient size disparity, suture tension, and time of complete suture removal are additional factors that have been shown to influence corneal radius of curvature after PKP, inducing high regular or irregular astigmatism. This represents another cause of visual impairment after PKP despite a clear corneal graft.7 After DALK surgery, a more regular corneal surface may be expected because of better donor-host conformity and the wider diameter of the grafts used.8 Post-DALK astigmatism has been reported to be less than or comparable with that associated with PKP.9,10
Several procedures have been proposed for remodeling and correction of high residual astigmatism (up to 5.00 D) after PKP. These have included selective suture removal, starting as early as 3 weeks postoperatively;11 relaxing incisions with or without compression sutures; wedge resections; arcuate keratotomy (AK); and toric phakic IOL implantation. Nevertheless, all of these procedures have presented limited and unpredictable effects, such as irregular induced astigmatism.8 AK incisions created with a femtosecond laser have offered a valid alternative to manual AK; however, this procedure is indicated only for astigmatism correction after keratoplasty, not for other types of residual refractive error.12
Similarly, for high residual myopic error correction, PRK, with or without mitomycin C application, has also been used; however, endothelial cell damage with mitomycin C and severe haze after PRK without mitomycin C have been noted as possible complications.13 LASIK after DALK was reported to have favorable efficacy outcomes, although undercorrection, decentered ablation, graft rejection related to excimer laser–induced inflammation, and regression were frequent complications.1 The introduction of the femtosecond laser for LASIK flap creation could potentially reduce flap-related complications.14 All procedures based on excimer laser ablation, however, include the risk of stromal inflammation, which may be an additional risk factor for graft rejection.15
A NEWER ALTERNATIVE
The absence of excimer laser ablation in small incision lenticule extraction (SMILE) may reduce PKP stromal inflammation and, consequently, the risk of graft rejection.16 Considering the safety, effectiveness, and broad application of this refractive procedure worldwide,16-23 since 2014, we have considered SMILE an option for treatment of myopic and/or astigmatic refractive error after DALK, in particular in patients who experience anisometropia or contact lens intolerance after the transplant surgery.24
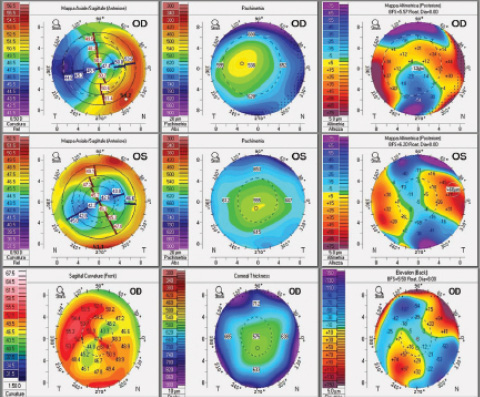
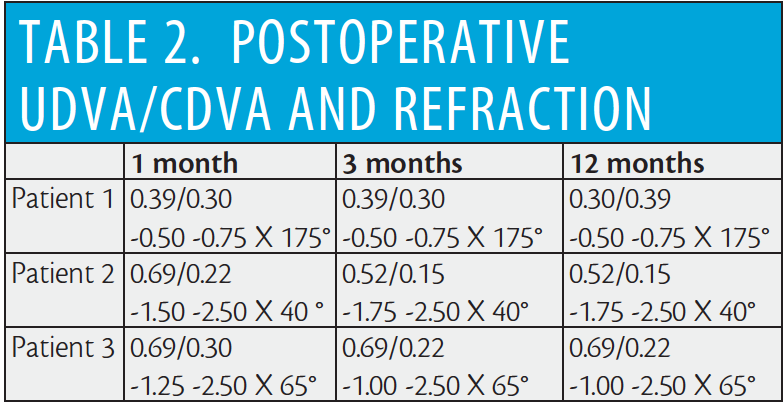
Figure 1. Preoperative topographic examinations in all patients showed moderate astigmatism, acceptable pachymetry, and normal posterior corneal surface elevation.
We have performed SMILE procedures after DALK in three keratoconus patients (Table 1). SMILE was performed at least 12 months after removal of all sutures to ensure that the refractive error was stabilized. Each patient had a transparent graft without dehiscence or other geometric alterations, documented with anterior segment OCT (AS-OCT; Optovue).
Preoperatively, patients underwent complete ocular examinations that confirmed absence of other ocular pathologies. Pentacam (Oculus) imaging showed a regular topographic corneal astigmatic pattern with a normal posterior corneal surface and an adequate corneal thickness (>500 µm) in each case (Figure 1). Objective and subjective refraction tests were performed, and UDVA and CDVA were recorded during preoperative visits in order to plan laser correction based on manifest refraction.
SURGICAL PROCEDURES
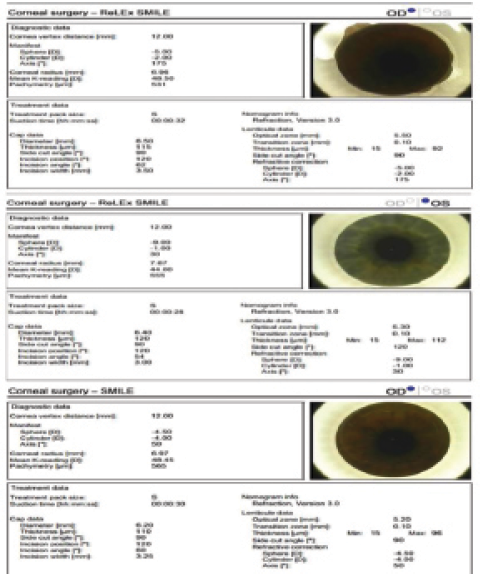
Figure 2. Surgical reports for three SMILE procedures after DALK.
Because all DALK grafts showed minimal decentration, the SMILE procedures were not centered on the graft but rather on the visual axis. The refractive corrections were chosen with consideration of the refraction in the patients’ contralateral eyes in order to reduce anisometropia (Figure 2).
VisuMax laser (Carl Zeiss Meditec) settings included laser cut energy of 150 mJ and spot spacing of 4 μm. SMILE was performed by an experienced surgeon (LM) with topical anesthesia achieved using oxybuprocaine tetrachloride applied repeatedly preoperatively. The femtosecond laser first created the lower interface of the intrastromal lenticule using an out-to-in direction to maximize the time that the patient’s central vision remained clear. Then the upper interface and sidecut were performed after the cap was sculpted. Finally, a 3.25-mm (60° arc length) superotemporal incision was created to link the cap interface to the corneal surface.25
All sculpted lenticules presented an oval profile because of the astigmatic portion of the treated refractive error. It was clear that both lenticules and incisions were contained within the limits of the graft.
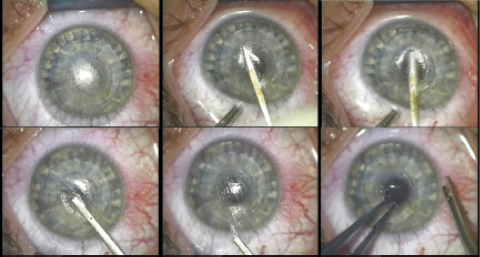
Figure 3. Lenticule separation and extraction: The small incision is opened and the upper and lower edges of the lenticule are delineated with a dedicated surgical instrument (A,B). Once both layers have been separated, a blunt spatula is inserted through the incision to separate and remove the refractive lenticule (C-E), which is then grasped with toothed forceps and evaluated by the surgeon to validate its shape and completeness (F).
Lenticule separation and extraction were performed under the surgical microscope. The small incision was opened and the upper and lower edges of the lenticule were delineated, in that order, with a dedicated surgical instrument. Once both layers had been separated, a blunt dedicated spatula was inserted through the incision to separate and allow removal of the refractive lenticule with toothed forceps (Figure 3).
Compared with a SMILE procedure in a normal cornea, a slightly greater difficulty was encountered by the surgeon in separation of the lenticule planes and removal of the lenticule, probably related to the difference in stromal tensile strength in a transplanted cornea between the graft and the recipient cornea.
POSTOPERATIVE FOLLOW-UP
The postoperative regimen included antibiotic and steroid eye drops. Follow-up examinations, including UCVA and BCVA, Pentacam tomography, AS-OCT, and in vivo confocal microscopy (IVCM; Retina Tomograph III, Heidelberg Engineering) were performed at 1 week and 1, 3, 6, and 12 months.
All patients reported only mild ocular discomfort and blurred vision during the first day after surgery. The postoperative course was uneventful, with no significant corneal inflammation and no signs of graft rejection or opacification.
Table 2 shows the refractive results during follow-up; UCVA and BCVA improved in all cases at 1 month postoperative, while refraction decreased and remained stable during follow-up. Topographic examinations showed improvement in central corneal regularity and reduction of topographic astigmatism; corneal thickness reduction was consistent with the thickness of the extracted lenticule, and posterior surface elevation did not show significant changes (Figure 4).
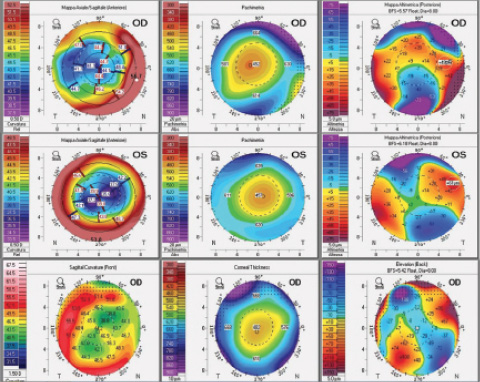
Figure 4. Postoperative topographic examinations showed evident improvement of central corneal regularity with reduction of topographic astigmatism; corneal thickness reduction as measured on topographic pachymetry maps was consistent with the thickness of the extracted lenticule, and the posterior corneal surface elevation did not show significant changes.
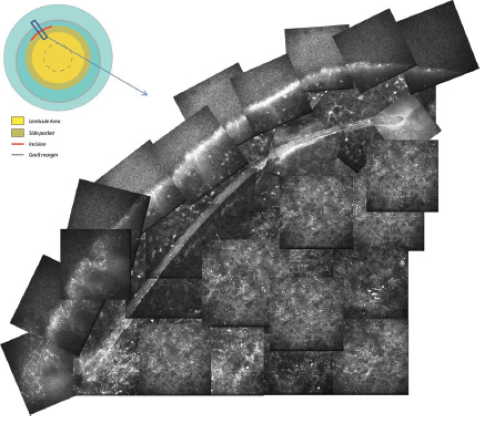
Figure 5. Graphical representation of a SMILE procedure after DALK (upper left): The lenticule area and the cap diameter were included within the graft margin, which is decentered with respect to the DALK centration. IVCM examination (lower right) of the small incision site showed (at stromal depth) an evident epithelial ingrowth at the incision site, near to the graft margin (superficial epithelial level).
IVCM examination of the small incision site showed, at stromal depth, evident epithelial ingrowth at the incision site, near to the graft margin (Figure 5), without any sign of tissue reaction or inflammation. Central corneal IVCM examination after surgery showed, in all patients, mild stromal interface edema and keratocyte activation at 1 week after surgery (Figure 6), immediately above and below the laser interface. This was no longer detectable after 3 months, when only minimal stromal keratocyte density reduction was evident at the laser interface.
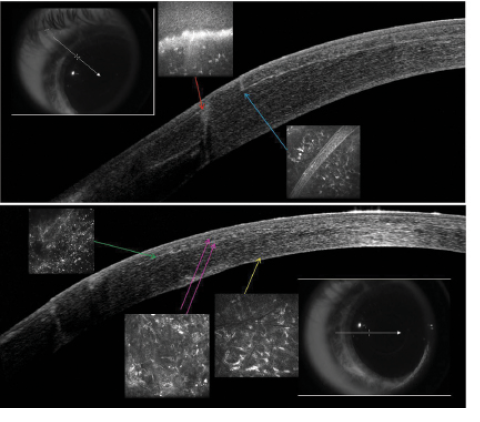
Figure 6. Top: AS-OCT examination and corresponding IVCM evaluations (insets) show graft margin (red arrow) and small incision (light blue arrow). Bottom: AS-OCT examination and corresponding IVCM images (insets) show femtosecond laser interface (green arrow) with superior and inferior stromal features (fuchsia arrow) and DALK interface (yellow arrow).
At 1 month, AS-OCT demonstrated two interface characteristics: the SMILE anterior lamellar interface (at approximately 110 µm below the corneal surface for all patients) and the DALK posterior pre-Descemetic interface (Figure 6).
Once adequate refractive stability was obtained, spectacle correction was prescribed for all patients.
CONCLUSION
In this article, we have described for the first time, to the best of our knowledge, application of SMILE in treatment of myopic symmetric astigmatism after DALK in a small series of patients. We have previously reported our experience in a single case report in the scientific literature.24 Our results to date suggest that this flapless, minimally invasive procedure can be used safely to correct residual refractive error in PKP eyes.
The results of the case series presented here show several advantages in the application of SMILE after DALK; from the first postoperative day and throughout follow-up, no symptoms of ocular discomfort or pain were reported, and no haze, graft rejection, or dry eye occurred. Reduction of tissue edema and inflammation were also confirmed by IVCM evaluation. Furthermore, no ectatic disorders of the posterior corneal surface developed in any of the three grafts (Figure 5); this is interesting, considering that the scientific literature presents conflicting opinions regarding the risk of keratectasia after SMILE.26,27
The posterior corneal surface, in our case series, did not appear to undergo substantial modifications, which supports the proposal that SMILE causes minimal damage to the deeper corneal layers,24 particularly in a transplanted cornea where a novel biomechanical equilibrium has been constituted.
The learning curve for SMILE is more difficult and longer for the surgeon, compared with that for standard refractive surgery. Nevertheless, the results seen in this series might lead surgeons to adopt this innovative refractive surgical procedure. Further prospective studies and larger case series are needed to demonstrate the long-term refractive outcomes of SMILE in PKP eyes.
1. Acar BT, Utine CA, Acar S, Ciftci F. Laser in situ keratomileusis to manage refractive errors after deep anterior lamellar keratoplasty. J Cataract Refract Surg. 2012;38(6):1020-1027.
2. Kim KH, Choi SH, Ahn K, Chung ES, Chung TY. Comparison of refractive changes after deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. Jpn J Ophthalmol. 2011;55(2):93-97.
3. Han DC, Mehta JS, Por YM, Htoon HM, Tan DT. Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2009;148(5):744-751.
4. Jones MN, Armitage WJ, Ayliffe W, Larkin DF, Kaye SB. Penetrating and deep anterior lamellar keratoplasty for keratoconus: a comparison of graft outcomes in the United Kingdom. Invest Ophthalmol Vis Sci. 2009;50(12):5625-5629.
5. Javadi MA, Feizi S, Rastegarpour A. Effect of vitreous length and trephine size disparity on post-DALK refractive status. Cornea. 2011;30(4):419-423.
6. Feizi S, Javadi MA. Factors predicting refractive outcomes after deep anterior lamellar keratoplasty in keratoconus. Am J Ophthalmol. 2015;160(4):648-653.
7. Shimmura S, Ando M, Ishioka M, Shimazaki J, Tsubota K. Same-size donor corneas for myopic keratoconus. Cornea. 2004;23(4):345-349.
8. Kubaloglu A, Coskun E, Sari ES, et al. Comparison of astigmatic keratotomy results in deep anterior lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2011;151(4):637-643.
9. Watson SL, Ramsay A, Dart JK, Bunce C, Craig E. Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004;111(9):1676-1682.
10. Ardjomand N, Hau S, McAlister JC, et al. Quality of vision and graft thickness in deep anterior lamellar keratoplasty and penetrating corneal allografts. Am J Ophthalmol. 2007;143(2):228-235.
11. Al-Torbak AA, Al-Motowa S, Al-Assiri A, et al. Deep anterior lamellar keratoplasty for keratoconus. Cornea. 2006;25:408-412,
12. Rückl T, Dexl AK, Bachernegg A, et al. Femtosecond laser-assisted intrastromal arcuate keratotomy to reduce corneal astigmatism. J Cataract Refract Surg. 2013;39(4):528-538.
13. Leccisotti A. Photorefractive keratectomy with mitomycin C after deep anterior lamellar keratoplasty for keratoconus. Cornea. 2008;27:417-420.
14. Aristeidou A, Taniguchi EV, Tsatsos M, et al. The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis (Lond). 2015;2:12.
15. Alio JL, Javaloy J. Corneal inflammation following corneal photoablative refractive surgery with excimer laser. Surv Ophthalmol. 2013;58(1):11-25.
16. Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism. Graefes Arch Clin Exp Ophthalmol. 2016;254(2):399-405.
17. Soong HK, Malta JB. Femtosecond lasers in ophthalmology. Am J Ophthalmol. 2009;147:189-197.
18. Zhao Y, Li M, Zhao J, et al. Posterior corneal elevation after small incision lenticule extraction for moderate and high myopia. PLoS One. 2016;11(2):e0148370.
19. Randleman JB, Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF. Depth-dependent cohesive tensile strength in human donor corneas: implications for refractive surgery. J Refract Surg. 2008;24(1):S85-89.
20. Li M, Zhao J, Shen Y, et al. Comparison of dry eye and corneal sensitivity between small incision lenticule extraction and femtosecond LASIK for myopia. PLoS One. 2013;8(10):e77797.
21. Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015;122(4):669-676.
22. Qian Y, Huang J, Zhou X, Wang Y. Comparison of femtosecond laser small-incision lenticule extraction and laser-assisted subepithelial keratectomy to correct myopic astigmatism. J Cataract Refract Surg. 2015;41(11):2476-2486.
23. Kobashi H, Kamiya K, Ali MA, Igarashi A, Elewa ME, Shimizu K. Comparison of astigmatic correction after femtosecond lenticule extraction and small-incision lenticule extraction for myopic astigmatism. PLoS One. 2015;10(4):e0123408.
24. Mastropasqua L, Calienno R, Lanzini M, Nubile M. Small incision lenticule extraction after deep anterior lamellar keratoplasty. J Refract Surg. 2015;31(9):634-637.
25. Reinstein DZ, Archer TJ, and Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes Eye Vis (Lond). 2014;1:3.
26. Remy M, Kohnen T. Corneal ectasia after femtosecond laser-assisted small-incision lenticule extraction in eyes with subclinical keratoconus/forme fruste keratoconus. J Cataract Refract Surg. 2015;41(7):1551-1552.
27. Sachdev G, Sachdev MS, Sachdev R, Gupta H. Unilateral corneal ectasia following small-incision lenticule extraction. J Cataract Refract Surg. 2015;41(9):2014-2018.
Roberta Calienno, PhD
• Fellow, National Centre of High Technology in Ophthalmology, University “G d’Annunzio,” Chieti-Pescara, Italy
• Financial interest: None acknowledged
Manuela Lanzini, PhD
• Fellow, National Centre of High Technology in Ophthalmology, University “G d’Annunzio,” Chieti-Pescara, Italy
• Financial interest: None acknowledged
Leonardo Mastropasqua, MD
• Head, National Centre of High Technology in Ophthalmology, University “G d’Annunzio,” Chieti-Pescara, Italy
• Financial interest: None acknowledged
Mario Nubile, PhD
• Researcher, National Centre of High Technology in Ophthalmology, University “G d’Annunzio,” Chieti-Pescara, Italy
• Financial interest: None acknowledged
