An IOL exchange is rarely required after modern cataract surgery owing to advances in surgical technique, IOL design, biometry, and lens calculation formulas.1,2 Nevertheless, IOL explantation and exchange are still sometimes required in certain situations. The first of these are lenticular problems such as IOL opacification, poor neural adaptation, and a damaged IOL. The second situation involves ocular problems such as IOL dislocation and decentration (Figure 1), capsular contraction, corneal decompensation, and IOL-related uveitis. An incorrect IOL power and toric IOL misalignment may also be indications for an IOL exchange.3 Iris-sutured and scleral-fixated IOLs are acceptable options for IOL exchange. Surgery requires an additional skill set.
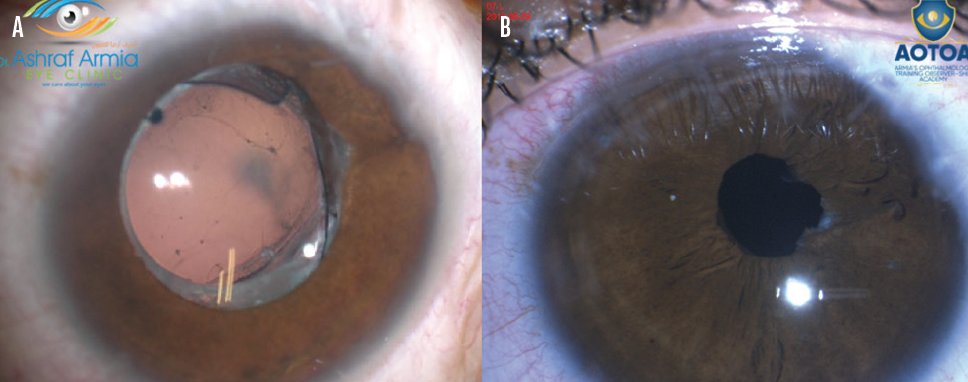
Figure 1. An IOL with the wrong power became displaced by vitreous strands with posterior synechiae (A). The IOL was exchanged for another lens. The pupil was nearly round after removal of all synechia, and the posterior chamber IOL was well centered in the sulcus (B).
This article presents details on several situations in which an IOL exchange is warranted and provides technical pearls.
WHEN TO CONSIDER IOL EXCHANGE
The most common indications. A dislocated IOL is the most common indication for an IOL exchange. The second most frequent indication is patient dissatisfaction after multifocal IOL implantation. Common reasons for dissatisfaction include asthenopia, positive dysphotopsias, residual refractive error, and uveitis-glaucoma-hyphema syndrome. (For more on this subject, see “When to Explant a Presbyopia-Correcting IOL and What to Put in Its Place"). Reasonable candidates for an IOL exchange are those with debilitating visual symptoms attributable to the IOL who have an intact posterior capsule and zonular support of the capsular bag.
Pediatric cataract surgery. Children who present for cataract surgery are at increased risk of axial length elongation, which predisposes them to a myopic shift.4 Should this occur, an IOL exchange is an option to reduce anisometropia and associated aniseikonia and to improve visual outcomes. This procedure is typically considered when a large myopic shift occurs in a pseudophakic child.
In my experience, IOL exchange in pediatric patients provides adequate visual rehabilitation (ie, decreased spectacle dependence and anisometropia) and a predictable postoperative refraction.
Children under the age of 7 months are at increased risk of requiring at least one additional intraocular surgery after the placement of a primary IOL. Informed consent for cataract surgery in this population should therefore discuss the risks with caregivers and prepare them for a long road ahead, including the likelihood that additional surgery will be required. Explaining that IOL exchange is a feasible solution to potential high myopia, especially in high-risk eyes, is important.5
IOL opacification. Glistenings found in the material of an IOL occur more frequently than IOL opacification, but neither usually causes a reduction in visual acuity significant enough to require an IOL exchange. A recent study, however, showed that certain procedures including Descemet stripping endothelial keratoplasty, Descemet stripping automated endothelial keratoplasty, Descemet membrane endothelial keratoplasty, and pars plana vitrectomy with intraocular gas or air injection predisposed lenses to opacification.6 The authors of that study also reported that opacification in the form of calcium precipitates on the IOL surface was more common with hydrophilic acrylic lenses(Figure 2; watch a related video on Eyetube), as were granular calcium deposits within the substance of the IOL optic, beneath the anterior surface of the lens optic, and in front of the posterior surface of the lens optic, the haptics, and the edge of the optic.
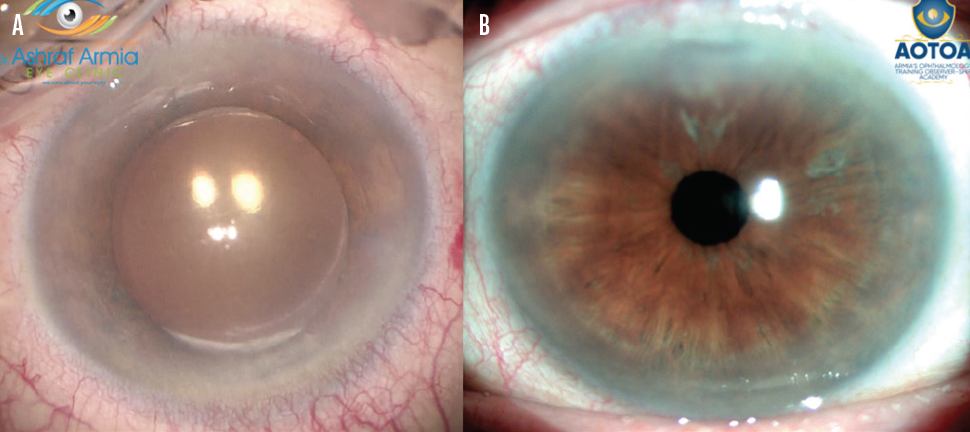
Figure 2. An opacified IOL (A) is removed and replaced despite the presence of an open posterior capsule. One month after surgery (B), BCVA was 20/20.
IOL opacification of any kind can significantly increase the amount of straylight and result in hazy vision and a poor quality of vision in dynamic lighting conditions. Straylight levels depend on the size and density of the opacification, which are determined by factors such as IOL material, manufacturing and packaging processes, concomitant ocular pathologies, and inflammatory factors.
The sooner opacification is identified, the more likely procedures such as an IOL exchange can be performed to ensure that vision quality is not affected. Anterior segment OCT is a reliable method to assess the presence, location, and density of changes to an IOL. Very superficial changes, however, may not be detectable.
SURGICAL STRATEGY
A scaffolding technique is one of the safest strategies to facilitate an IOL exchange, and it is often used in patients presenting with visual complaints attributed to a refractive surprise or dissatisfaction with the optical performance of an IOL.5 A scaffolding technique involves the manipulation of the original IOL out of the capsular bag and into the anterior chamber and the insertion of a replacement IOL into the capsular bag. The anteriorly elevated original IOL is transected with the IOL cutters while the new IOL acts as a scaffold for the posterior capsule. The continuous distension of the capsular bag prevents damage to the posterior capsule, and the replacement IOL acts as a barrier to vitreous prolapse. It also prevents slippage of the optic while pieces of the original IOL are removed.
This technique does not require enlargement of the corneal incision to facilitate explantation of the transected IOL. Attention, however, should be paid to possible adhesions between the IOL haptic and the capsule.
In eyes with an open posterior capsule, sulcus fixation of a three-piece IOL can be considered. In eyes with no capsular support, a modified technique is required. A scleral-fixated IOL is one option. Sutureless scleral fixation eliminates suture-related complications and can provide a high-quality functional outcome. Another option is the four-flanged technique, which can improve and simplify the intrascleral fixation of a one-piece, nonfoldable IOL. Additional options are the retropupillary placement of an Artisan IOL (Ophtec) and an iris-sutured three-piece IOL.
COMPLICATIONS
Serious complications, though rare, can occur with an IOL exchange, and informed consent requires a thorough discussion of the risks.
Intraoperative complications include vitreous loss, posterior capsular rupture, and an anterior extension of the capsulorhexis. An anterior vitrectomy for vitreous loss, placement of a capsular tension ring, and suturing of incisions may be required.
Postoperative complications include wound leak, recurrent vitreous hemorrhage, IOL tilt, and posterior capsular opacification. Resuturing the incision, repositioning the IOL, and an Nd:YAG laser capsulotomy or scanning laser trabeculoplasty may be required.7 (For more on Nd:YAG laser capsulotomy, see “When To YAG and When Not To".)
CONCLUSION
IOL repositioning is more cost-effective than IOL exchange, but the duration of the latter procedure is shorter. Cost-efficiency is not a sufficient reason to recommend IOL repositioning instead of IOL exchange.8 A greater ability to place an intracapsular IOL with few intraoperative complications and largely treatable postoperative complications enhances the effectiveness of IOL exchange and patient satisfaction. Although a challenging procedure, IOL exchange is a valuable treatment option for a broad spectrum of problems.
1. Abdalla Elsayed MEA, Ahmad D, Al-Abdullah AA, et al. Incidence of intraocular lens exchange after cataract surgery. Scientific Reports. 2019;9:12877.
2. Oltulu R, Erşan I, Satirtav G, Donbaloglu M, Kerimoğlu H, Özkağnici A. Intraocular lens explantation or exchange: indications, postoperative interventions, and outcomes. Arq Bras Oftalmol. 2015;78(3):154-157.
3. Goemaere J, Trigaux C, Denissen L, et al. Fifteen years of IOL exchange: indications, outcomes, and complications.
J Cataract Refract Surg. 2020;46:1596-1603.
4. Kraus CL, Trivedi RH, Wilson ME. Intraocular lens exchange for high myopia in pseudophakic children. Eye. 2016;30:1199-1203.
5. Narang P, Steinert R, Little B, Agarwal A. Intraocular lens scaffold to facilitate intraocular lens exchange. J Cataract Refract Surg. 2014;40:1403-1407.
6. Grzybowski A, Markeviciute A, Zemaitiene R. A narrative review of intraocular lens opacifications: update 2020. Ann Transl Med. 2020;8(22):1547.
7. Jones JJ, Jones YJ, Jin GJC. Indications and outcomes of intraocular lens exchange during a recent 5-year period. Am J Ophthalmol. 2014;157:154-162.
8. Kristianslund O, Dalby M, Moe MC, Drolsum L. Cost-effectiveness analysis in a randomized trial of late in-the-bag intraocular lens dislocation surgery: repositioning versus exchange. Acta Ophthalmol. 2019;97:771-777.