

Intraocular Lens Power Calculation in Eyes With Keratoconus
Savini G, Abbate R, Hoffer KJ, et al1
Industry support: K.J.H. licenses registered trademark name Hoffer to various companies
ABSTRACT SUMMARY
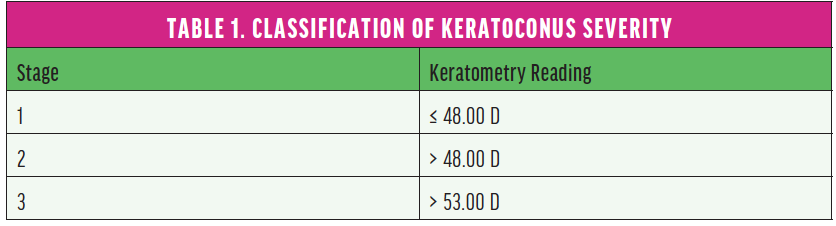
Savini and colleagues compared the prediction errors (PEs) of five standard formulas: Barrett Universal II (BUII), Haigis, Hoffer Q, Holladay 1, and SRK/T. The study included 41 consecutive keratoconic eyes undergoing phacoemulsification and IOL implantation. Eyes were classified by disease severity (Table 1).
A subjective refraction was obtained for each eye at 1 month postoperatively. The PE for each eye was calculated by subtracting the predicted spherical equivalent from the actual postoperative spherical equivalent. Myopic and hyperopic surprises were indicated by negative and positive PEs, respectively. Mean error (ME), median absolute error (MedAE), mean absolute error, and percentage of eyes achieving within ±0.50 D, ±0.75 D, and ±1.00 D of the refractive target were also calculated.
Study in Brief
A multicenter retrospective study compared the prediction errors of five standard formulas for IOL power calculation in eyes with keratoconus. Even with the most accurate of these formulas, refractive outcomes were significantly worse than those achieved in healthy eyes.
WHY IT MATTERS
IOL power calculations are less accurate for eyes with keratoconus, and hyperopic refractive surprises are commonplace. This is the first study to assess the accuracy of the Barrett Universal II for keratoconic eyes.
A hyperopic ME was found across all five formulas. Across the whole dataset, the lowest ME (0.91 D) and MedAE (0.62 D) and the highest percentage (36%) of eyes within ±0.50 D of target were achieved with the SRK/T formula. Outcomes were best among eyes with stage 1 disease. Accuracy decreased with more advanced keratoconus, with a MedAE of greater than 2.50 D in all stage 3 eyes.
DISCUSSION
Keratoconus presents multiple challenges to IOL selection. First, the standard keratometric index cannot reliably be applied to these eyes because this index depends on a normal ratio between the anterior and posterior corneal surfaces, but this ratio is disrupted in keratoconus. Second, keratometry assumes a degree of consistency in corneal curvature along any given meridian, which is not true for keratoconic eyes with asymmetrical corneal curvature. Third, standard IOL formulas predict the effective lens position based on theoretical model eyes and data obtained from normal eyes. The increased corneal curvature, axial length, and anterior chamber depth typical of keratoconic eyes and the abnormal relationships between these parameters limit the applicability of standard formulas. Fourth, tear film irregularities restrict the repeatability of corneal measurements, thereby introducing an additional source of error.
As a consequence, hyperopic refractive surprises after cataract surgery are commonplace among keratoconic eyes when IOL selection is based on traditional formulas.2 The accuracy of IOL calculations in keratoconus remains significantly worse than in normal eyes, of which 80% to 90% achieve within ±0.50 D of the refractive target when the latest methods are used.
Several formulas have been shown to provide greater accuracy than the older SRK/T formula for IOL power calculations in normal eyes and those with abnormal axial lengths and other abnormal biometric parameters. The BUII, for example, is one of the best-performing formulas in nonkeratoconic eyes, but it failed in this study to match the accuracy of the SRK/T formula in keratoconic eyes.
This study corroborates three conclusions drawn by other researchers:
- There is a strong tendency toward hyperopic PE in keratoconic eyes;2
- Greatest accuracy in this population is achieved by using the SRK/T formula;3 and
- IOL formula accuracy is inversely proportional to keratoconus severity.4
Savini et al offer a possible explanation for the greater accuracy of the SRK/T formula: In healthy eyes with steep corneas, this formula is less accurate and overestimates IOL power, leading to myopic surprises. This flaw is counterbalanced by the tendency toward hyperopic surprises in keratoconic eyes. It is therefore through serendipity rather than design that the SRK/T achieves superiority.
Aside from its small sample size (N = 41), other limitations of this study must be acknowledged. Disparate biometry methods and IOL models were employed across the different sites. Importantly, some preoperative data (eg, lens thickness) were lacking, precluding an investigation of formulas that require this information. Although the BUII may be used with just two or three parameters, it performs best with its full complement of five (keratometry, axial length, anterior chamber depth, lens thickness, and white-to-white distance). This is particularly true in abnormal eyes, for which the additional parameters improve accuracy. Thus, this study might have underestimated the efficacy of the BUII.
Accuracy of Intraocular Lens Power Formulas Modified for Patients With Keratoconus
Kane JX, Connell B, Yip H, et al5
Industry support: None
ABSTRACT SUMMARY
This retrospective study compared the accuracy of two IOL power formulas modified specifically for patients with keratoconus (Holladay 2 with keratoconus adjustment and Kane keratoconus formula [Kane-KC]) to seven normal IOL power formulas (BUII, Haigis, Hoffer Q, Holladay 1, Holladay 2, Kane, and SRK/T). (Editor’s note: J.X.K. devised the Kane and Kane-KC formulas.)
Study in Brief
A retrospective consecutive case series compared the accuracy of IOL power formulas modified specifically for patients with keratoconus to normal IOL power calculations. One of the modified formulas was found to be the most accurate for this patient population.
WHY IT MATTERS
This is the first study to evaluate IOL power formulas modified specifically for patients with keratoconus.
The Kane-KC achieved the lowest mean absolute error (0.81 D, P < .01) and MedAE (0.50 D) and the highest percentage (50%) of eyes within ±0.50 D of the refractive target across all stages of keratoconus using the same classification system as Savini et al (shown in Table 1).1 This was statistically significant when compared to the other formulas. Furthermore, the Kane-KC achieved an ME of just 0.04 D, whereas the other formulas returned hyperopic MEs ranging from 0.31 D (SRK/T) to 0.78 D (Hoffer Q).
Despite the greater accuracy of the Kane-KC, the accuracy of outcomes did not approach that expected in normal eyes. The Holladay 2 with keratoconus adjustment was the least accurate of the formulas investigated. All normal formulas resulted in a hyperopic ME that worsened with increasing keratometry.
DISCUSSION
This study supports previous findings that the SRK/T is the most accurate of the traditional formulas for eyes with keratoconus, followed by the BUII and original Kane formulas, which returned similar outcomes. These remain the best of a bad bunch, however, because only approximately 40% to 45% of keratoconic eyes were within ±0.50 D of target compared to an anticipated 80% or more in normal eyes.
This study found the Kane-KC to be a better option than any of the standard formulas investigated. Although the Kane-KC represented a welcome, statistically significant improvement, results were far inferior to the accuracy achieved in normal eyes. Further work to improve the accuracy of IOL power calculation for eyes with keratoconus is necessary. The recently released keratoconus modification of the True K formula, devised by Graham D. Barrett, MB BCh SAf, FRACO, FRACS, and available for free from the Asia-Pacific Association of Cataract & Refractive Surgeons (www.apacrs.org), is therefore of great interest. In a recent personal communication to one of the authors (A.M.J.T.), Dr. Barrett stated that early results suggest that this modified formula holds great promise.
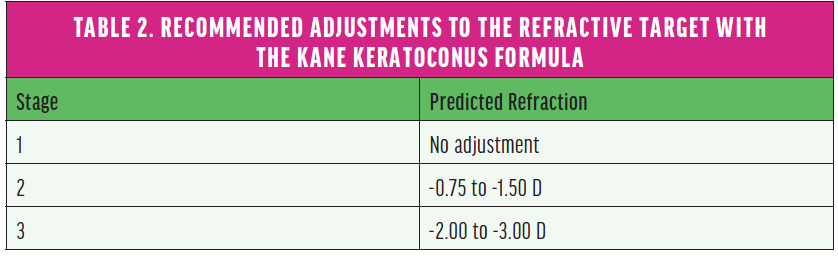
To further optimize outcomes and avoid hyperopic errors after cataract surgery on eyes with keratoconus, Kane et al recommend adjusting the refractive target when using the Kane-KC (Table 2).
1. Savini G, Abbate R, Hoffer KJ, et al. Intraocular lens power calculation in eyes with keratoconus. J Cataract Refract Surg. 2019;45(5):576-581.
2. Kamiya K, Iijima K, Nobuyuki S, et al. Predictability of intraocular lens power calculation for cataract with keratoconus: a multicenter study. Sci Rep. 2018;8(1):1312.
3. Hashemi H, Heidarian S, Seyedian MA, Yekta A, Khabazkhoob M. Evaluation of the results of using toric IOL in the cataract surgery of keratoconus patients. Eye Contact Lens. 2015;41(6):354-358.
4. Watson MP, Anand S, Bhogal M, et al. Cataract surgery outcome in eyes with keratoconus. Br J Ophthalmol. 2014;98(3):361-364.
5. Kane JX, Connell B, Yip H, et al. Accuracy of intraocular lens power formulas modified for patients with keratoconus. Ophthalmology. 2020;127(8):1037-1042.



