
I encounter negative dysphotopsia (ND) often in my practice. Patients typically describe this visual phenomenon as a dark, temporal crescent in the far periphery of an eye that had uneventful cataract surgery.
I try to acknowledge patients’ symptoms by telling them that about 10% of people see this dark shadow on the first postoperative day. This number drops to about 0.5% (1 in 200) by 6 months postoperative.1 I tell patients to let me know if they still notice it in 6 months, and, if they do, we can take care of it. This reassurance stops most patients from fixating on the issue. It seems the more they ignore it, the more likely they will neurally adapt to the ND.
At a Glance
• Although eyes with ND typically have normal visual acuity, patients experiencing this visual phenomenon describe it as a dark, temporal crescent in the far periphery of the eye.
• If symptoms of ND persist months after surgery, encourage the patient to wear thick-rimmed glasses, as the rim seems to cover up the symptoms.
• Whether caused by a shadow cast from the nasal anterior capsule or caused by a gap between the light rays passing anterior to the IOL and those passing through the posterior IOL, ND is definitively treated by moving the IOL optic anterior to the nasal capsular edge.
CONSIDERATIONS BEFORE TREATMENT
If symptoms persist months after surgery, I first obtain a visual field to rule out a neurologic issue. I have never found any. I encourage the patient to wear thick-rimmed glasses because the rim seems to cover up the symptoms, perhaps by decreasing stray light from the temporal side. Such light seems to make symptoms worse.
Eyes with ND typically have normal visual acuity. Before I am ready to operate, I encourage the patient to have cataract surgery on the other eye first. Why take a risk to treat the 20/20 first eye until we know that the second eye has successfully undergone cataract surgery without postoperative complications?
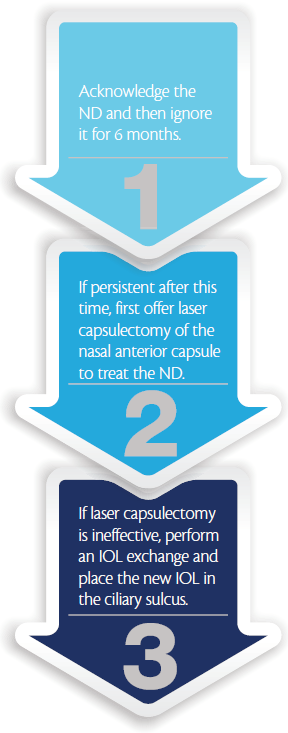
Algorithm for Treating ND
Although ND has been associated with several IOL types, if the patient has complaints with one IOL type, I try to move to a completely different style of IOL for the other eye. For example, if the patient had an acrylic, one-piece IOL with square optic edges in the first eye, I might choose a silicone, three-piece IOL with rounded optic edges for the second eye. Also, it makes good sense to perform reverse optic capture of the IOL in the second eye.
TWO TYPES OF ND
There seem to be two types of ND. One type is ameliorated by Nd:YAG laser capsulectomy of the nasal anterior capsule. My suspicion is that this first type is caused by a shadow cast from the nasal anterior capsule.2 The other type of ND is cured by decreasing the space between the IOL and the iris. This type of ND occurs when light rays passing through the peripheral edge of the IOL are refracted posterior to those passing through the posterior surface, creating a shadow between them.3
Either type of ND is definitively treated by moving the IOL optic anterior to the nasal capsular edge. If a patient is highly troubled by ND, I go straight to this procedure. Masket and Fram describe moving the IOL anteriorly and keeping the haptics in the bag, and they call this procedure reverse optic capture.2 I usually perform an IOL exchange and place the new lens in the ciliary sulcus. First, however, I offer laser.
Ignore the ND
• Approximately 10% of people have ND on postoperative day 1.
• The ND remains noticeable in about 0.5% of people (1 in 200) by 6 months postoperative.
• Getting patients to stop fixating on the ND can be challenging. One strategy is to tell patients to report ND if they still notice it after 6 months and, at that time, it will be addressed.
LASER TREATMENT
In some patients, ND is completely cured by Nd:YAG laser nasal anterior capsulectomy, whereas others are not helped at all. I typically ask the patient with bothersome ND to consider Nd:YAG laser repair prior to surgical repair.
Although moving the IOL to the sulcus always fixes ND, using the Nd:YAG laser often fixes it, and the procedure is easy to do. Aiming at the anterior capsule, I always fear pitting the IOL, but that has happened only once, and damage was minimal. I start with low power, aiming anterior to the IOL in an area that will be covered by an undilated pupil. I move toward the anterior capsule and increase the power until I make a small opening. I try to stay in this plane until I have cut a section of the capsule free.
During the procedure, I try to blow the capsule piece into the sulcus, so to speak. Although, on occasion, capsule pieces have fallen into the inferior angle, I have never identified any problems from these pieces. I avoid opening the posterior capsule because some of these eyes will require surgical IOL manipulation to alleviate the ND.
SURGICAL TREATMENT
In patients who require surgery, I have been amazed at how easily typically shaped IOLs can be viscodissected from the capsular bag. I have encountered difficulty with only one IOL, which had fixation holes. The anterior and posterior capsules were highly adherent to each other within these holes.
Removing the IOL is easy, as long as care is taken to completely viscodissect the haptics. I have removed two IOLs in which a previous posterior capsulotomy was performed elsewhere. In one of those cases, I was able to avoid vitrectomy by slowing down and remembering my own dictum: Never tug on the IOL. Rather, if the IOL does not move easily, I use more OVD.
To remove the IOL, I use a 3-mm incision. Before surgery, I mark any place where a gap appears under the anterior capsule; I place a paracentesis track opposite that mark to facilitate placing OVD at the site. Even if no capsule opening is obvious, one can be created by indenting the IOL with a sharp Sinskey hook; Samuel Masket, MD, has suggested a 30-gauge needle for this. This maneuver allows me to get under the capsule. I then hold the gap open and inject OVD.
Even capsule-to-capsule adhesions that have been present for years can be separated with OVD. The wave of viscoelastic material carries beyond the bag equator and can be seen traveling behind the IOL. Once the IOL is free of adhesions, I rotate it into the sulcus and externalize one haptic. I cut and hold the IOL—either by the haptic or by the optic—through the same incision. My best two instruments for grasping the IOL optic are Packer/Chang microforceps (MicroSurgical Technology) or Utrata forceps. The Packer/Chang IOL cutter (MicroSurgical Technology) is wonderful for cutting the IOL. After the optic is bisected, the two pieces are easily removed and the new IOL is placed in the sulcus.
SUMMARY
If a patient complains of ND, I acknowledge it and then ignore it for 6 months. If ND persists after this time, I first offer laser capsulectomy of the nasal anterior capsule; if this is not effective, I follow it with IOL exchange, placing the new IOL in the ciliary sulcus. I have found this algorithm to be an effective and satisfying way to deal with this unwanted visual phenomenon. n
1. Bournas P, Drazinos S, Kanellas D, et al. Dysphotopsia after cataract surgery: comparison of four different intraocular lenses. Ophthalmologica. 2007;221(6):378-383.
2. Masket S, Fram NR. Pseudophakic negative dysphotopsia: surgical management and new theory of etiology. J Cataract Refract Surg. 2011;37:1199-1207.
3. Holladay JT, Zhao H, Reisin CR. Negative dysphotopsia: the enigmatic penumbra. J Cataract Refract Surg. 2012;38:1251-1265.
David L. Cooke, MD
• Clinical Assistant Professor, Department of Neurology and Ophthalmology, Michigan State University, College of Osteopathic Medicine, East Lansing, Michigan
• dcooke@greateyecare.com
• Financial Disclosure: None

