
With the emergence of corneal inlays for the correction of presbyopia, there has been debate on how to implant these devices into the cornea. Of the four inlays on the market, the manufacturers of three of them recommend implanting intrastromally—in a corneal pocket—and one is designed for implantation under a flap.
The initial recommendation for the Kamra inlay (AcuFocus), which uses the pinhole effect to create depth of focus in the implanted eye, was to implant it under a 200-µm flap. However, the location for implantation was subsequently switched to an intrastromal pocket, where the device could be implanted deeper to improve its safety and efficacy. AcuFocus now recommends a pocket 200 to 250 µm deep, created with a femtosecond laser using the manufacturer’s guidelines for settings to achieve the best possible pocket with the smoothest stromal bed. This setting can vary from laser to laser, and it may be that certain femtosecond lasers yield better results than others.
The Icolens (Neoptics) and the Flexivue (Presbia) are both implanted intrastromally as well, at a depth of 300 µm into the cornea. These inlays have refractive power, and they split the incoming light to create multifocality on the retina. The inlays look like a donut, with a 3.6-mm diameter. Flexivue claims there is no keratocyte activity with the implant at a depth of 300 µm, thus reducing haze and the need for biocompatibility of the material.
The Raindrop Near Vision Inlay (ReVision Optics) is the only inlay that is currently recommended to be implanted under a flap. The flap is a standard 8- to 9-mm LASIK flap created at a depth of about 30% of central corneal thickness. The flap thickness should be a minimum of 150 µm, but typically I create a 170 to 180 µm flap, depending upon the thickness of the cornea.
POCKET VERSUS FLAP
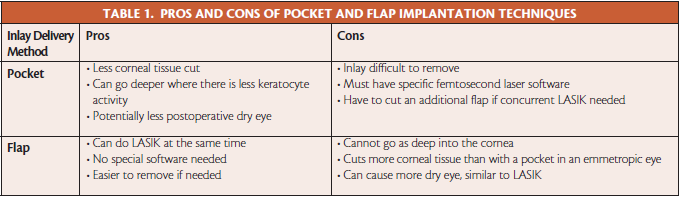
I have experience with the Kamra and the Raindrop, but not with the two PMMA devices. I have done flaps and pockets for the Kamra and flaps for the Raindrop, although it should be noted that I have not performed large numbers of procedures with either implant to date. My experience dictates that there are pros and cons to each delivery method (Table 1) but that, ultimately, what matters is that the inlay performs safely and effectively within the cornea.
Because the inlays are made out of different materials, they behave differently in the cornea. Each has its own inherent drawbacks and benefits for certain patients. For example, if a patient’s refraction is naturally around -0.75 D, the Kamra is better suited; if the patient is between plano and 1.50 D, the Raindrop suits better.
My impression is that I have seen more consistent results, earlier patient satisfaction, and fewer unwanted symptoms with the Raindrop inlay. I have not seen a difference in postoperative dry eye between the two inlays. Both the Kamra and the Raindrop are straightforward to use. The hydrogel material (made of 80% water) of the Raindrop is biocompatible, works well under a flap, and should work well in a pocket, too. Variable performance was reported with the Kamra under flaps, and hence the company now endorses Kamra inlay implantation only in pockets. They have introduced the concept of planned LASIK Kamra in two steps, a procedure referred to as PLK2.
CONCLUSION
One important feature of all corneal inlays is that they are removable. If the patient does not like his or her outcome, or if I feel that the inlay is not being well tolerated, then I can remove it from inside the pocket or under the flap. My gut feeling is that all inlays will ultimately do better implanted intrastromally in a pocket, so I am hopeful that this will be a possibility with the Raindrop device in the future. n
Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
• Consultant Ophthalmologist, Wellington Eye Clinic and Beacon Hospital, Dublin, Ireland
• Associate Chief Medical Editor, CRST Europe
• abc@wellingtoneyeclinic.com
• Financial disclosure: Consultant (Alcon, WaveLight) Past financial compensation (ReVision Optics)
