In response to the US Centers for Disease Control and Prevention’s recommendation, the use of face masks has risen dramatically in the United States.1 The prevalence of dry eye disease (DED) and ocular irritation has risen concurrently.2 The phenomenon of mask-associated dry eye (MADE), its prevalence, and associated factors require a full assessment and treatment before corneal refractive or cataract surgery.
CAUSES
Wearing face masks is essential to combatting the spread of SARS-CoV-2, but prolonged wear has increased the prevalence of DED.3 MADE has affected much of the US population,2 and the likely cause is changing airflow dynamics. Face masks reduce the outward spread of air and direct it upward toward the eyes.3 As this air stream travels over the corneal surface, it accelerates tear film evaporation, drying the ocular surface and causing discomfort in both patients with no history of DED and those with preexisting disease. Additionally, increased face touching and eye rubbing as reactions to an ill-fitting mask can lead to infection, an allergic response, and further dysregulation of the tear film.3
Groups at particularly high risk for MADE include contact lens wearers, postmenopausal women, and individuals with known connective tissue or autoimmune diseases. Other groups at risk include individuals in professions that require prolonged mask wear and/or long hours of digital device use. The Figure depicts three solutions that patients can consider to reduce the symptoms of DED.
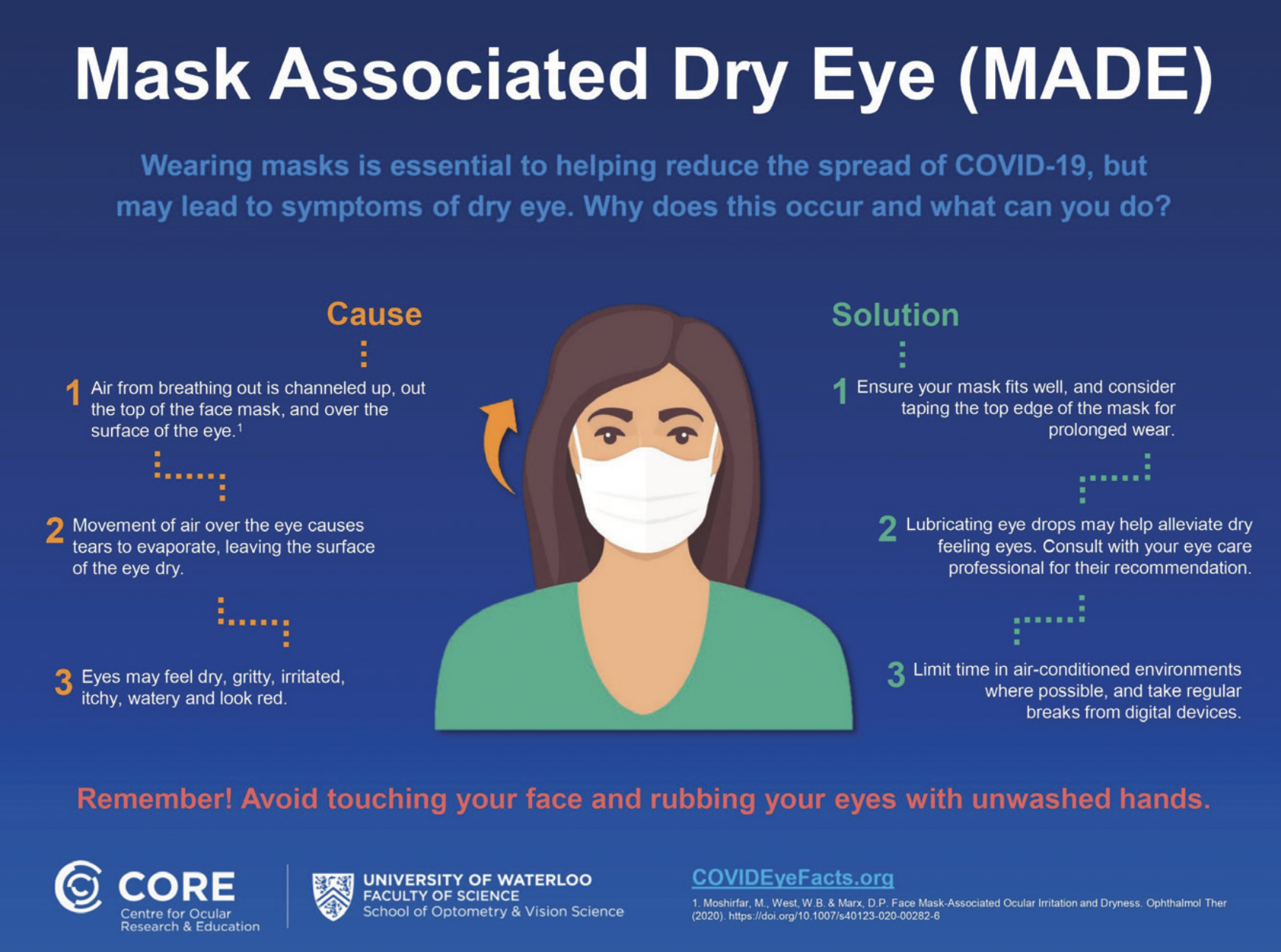
Figure. Causes of and solutions for MADE.
PREVALENCE
Many eye care practitioners have anecdotally reported an increase in DED symptoms among their patients in the past year-plus. A cross-sectional study measured self-reported symptoms of MADE in the general population in an effort to identify factors influencing the condition (eg, age, sex, occupation, and the use of refractive correction in the form of glasses or contact lenses).4
A total of 3,605 survey responses from participants aged 11 to 88 years were analyzed. More than half (54.3%) said they sometimes experienced DED symptoms, and 13.6% said they often experienced DED symptoms. The remaining 32.1% said they never experienced DED symptoms. Of the 2,447 individuals who reported experiencing symptoms, 658 (26.9%) said the symptoms worsened when a face mask was worn, meaning 18.3% of the entire sample experienced MADE. Women were more likely than men to report ocular irritation and worsened DED symptoms due to wearing a face mask.
Interestingly, there were no statistically significant differences in discomfort level between contact lens wearers and individuals who wore glasses, but participants who did not wear a form of vision correction reported less frequent symptoms. Similarly, perceived worsening of symptoms did not differ between individuals who wore contact lenses and those who wore glasses, but participants who reported the use of no vision correction experienced MADE less frequently.
IMPACT ON CORNEAL AND LENS-BASED REFRACTIVE SURGERY
A healthy ocular surface is essential to achieving the best visual outcomes after surgery.5 Patients’ use of face masks immediately before and after corneal and lens-based refractive procedures is therefore of concern. Before the COVID-19 pandemic, the Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study found that 77% of patients being evaluated for cataract surgery had corneal staining and 63% had an unstable tear film (rapid tear breakup time).6 In a 2015 study, my colleagues and I found significantly greater variability in average keratometry readings and anterior corneal astigmatism among patients with tear hyperosmolarity. As a result, there was a higher probability of an error of 1.00 D or more in the IOL power calculation.7
The prevalence of MADE exacerbates this situation. Eye care providers must be vigilant in their assessment of the ocular surface and tear film.
CASE REPORT
At least one case of acute postoperative MADE has been reported in the peer-reviewed literature.8 A 66-year-old woman with a history of LASIK for high myopia underwent routine cataract surgery. Postoperatively, the cornea looked clear, and the patient reported clear vision. As was standard practice, the staff placed a clear plastic shield over the patient’s eye and replaced her face mask postoperatively.
A few hours later, the patient returned with discomfort and blurry vision. There was no evidence of intraocular inflammation, and the LASIK flap was undisturbed. Corneal haze was widespread, and there was superficial staining with topical fluorescein. UCVA decreased to counting fingers, and pinhole acuity was 20/32.
Further examination found the ocular surface of the operated eye to be extremely dry compared with that of the unoperated eye. The patient’s face mask was observed to fit loosely around her nose. She was advised to minimize her use of a face mask when possible and to continue with the prescribed postoperative regimen of steroid and antibiotic drops. Two days later, UCVA was 20/25. At 1 week, the cornea was clear with no evidence of DED.
Chadwick and Lockington concluded that a poor-fitting face mask was to blame for this unique case.8 As the basis of their conclusion, they cited other conditions under which improper airflow leads to exposure keratopathy. For example, patients who use continuous positive airway pressure (CPAP) ventilation or another nasal mask therapy device may be at risk of ocular irritation secondary to airflow from mask leakage or retrograde nasolacrimal air escape—especially if they are new users.9-11 Compared to the general US adult population, the incidence of DED is higher in patients who use CPAP and nasal mask therapy devices. The incidence of DED also increases based on the length of time a CPAP device is used.12
CONCLUSION
A surge in the use of face masks has increased the incidence of DED and ocular irritation. As more of patients experience MADE, clinicians must be more diligent about assessing the ocular surface and tear film before corneal refractive or cataract surgery. Clinicians are fortunate already to have extensive knowledge about diagnosing and treating DED. Now, those skills must be put to greater use in the months and years ahead.
1. Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff. 2020;39:1419-1425.
2. Moshirfar M, West WB Jr, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9(3):397-400.
3. Pandey SK, Sharma V. Mask-associated dry eye disease and dry eye due to prolonged screen time: are we heading towards a new dry eye epidemic during the COVID-19 era? Indian J Ophthalmol. 2021;69(2):448-449.
4. Boccardo L. Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people. Published online January 20, 2021. Cont Lens Anterior Eye. doi:10.1016/j.clae.2021.01.003
5. Movahedan A, Djalilian AR. Cataract surgery in the face of ocular surface disease. Curr Opin Ophthalmol. 2012;23(1):68-72.
6. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
7. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41:1672-1677.
8. Chadwick O, Lockington D. Addressing post-operative mask-associated dry eye (MADE). Published online November 13, 2020. Eye (Lond). doi:10.1038/s41433-020-01280-5
9. Kadyan A, Asghar J, Dowson L, Sandramouli S. Ocular findings in sleep apnoea patients using continuous positive airway pressure. Eye (Lond). 2010;24(5):843-850.
10. Stauffer JL, Fayter N, MacLurg BJ. Conjunctivitis from nasal CPAP apparatus. Chest. 1984;86(5):802.
11. Fayers T, Simcock DE, Wilkins MR. Reactivation of recurrent corneal erosion syndrome by continuous positive pressure ventilation. Cornea. 2007;26(10):1292.
12. Matossian C, Song X, Chopra I, Sainski-Nguyen A, Ogundele A. The prevalence and incidence of dry eye disease among patients using continuous positive airway pressure or other nasal mask therapy devices to treat sleep apnea. Clin Ophthalmol. 2020;14:3371-3379.



