CASE PRESENTATION
A 52-year-old woman presents with a complaint of dysphotopsias—glare and shadows—that are especially noticeable in dim lighting conditions.
The patient received an Artisan IOL (Ophtec) in each eye 15 years ago for the treatment of high myopia. Both eyes subsequently developed a cataract, which necessitated removal of the phakic IOLs. Phaco cataract surgery and IOL implantation were carried out elsewhere. The procedure on the dominant right eye was routine. Surface ablation was performed to address a myopic refractive surprise, after which uncorrected distance visual acuity was 6/5. Cataract surgery on the left eye was complicated by rupture of the posterior capsule. A three-piece IOL was placed in the sulcus. This eye underwent surface ablation to address a myopic refractive surprise, after which uncorrected distance visual acuity was 6/7.5, which did not improve with refraction.
On examination, the right eye is normal, and the Figure shows the left eye. Corneal topography and the tear film are normal in each eye. The rest of the ocular examination is unremarkable.
How would you proceed?
—Case prepared by Allon Barsam, MD, MA, FRCOphth
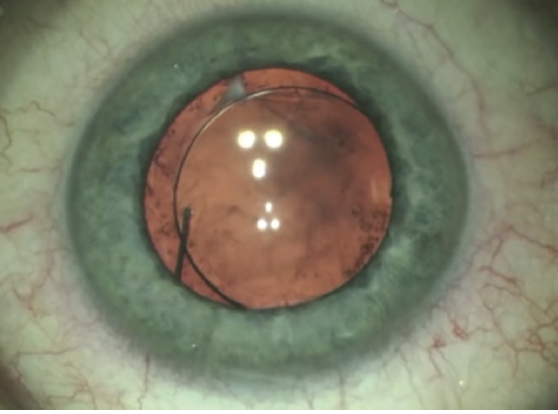
Figure. Anterior segment of the left eye.

ARTHUR B. CUMMINGS, MB CHB, FCS(SA), MMED(OPHTH), FRCS(EDIN)
I am assuming that the only issue in play here is the decentered three-piece IOL that is fixated in the sulcus, given that the rest of the ocular examination is reportedly unremarkable. The decentered IOL is the likely cause of the dysphotopsias. Management includes recentration of the IOL optic.
Further surgery will determine whether the IOL can simply be repositioned by rotating from the current position if the haptics are intact. I cannot see the edges of the capsulorhexis in the Figure, but, if the capsulorhexis is well centered, optic capture can readily resolve the issue.
Capsular fibrosis at the 11 clock position may be the cause of decentration, and this requires exploration. Using an OVD, the optic would be placed over the fibrosed area or, better yet, excised or released if it is the culprit. The possible tilt of the IOL, as indicated by the misaligned Purkinje reflexes, suggests that the haptics may be in the sulcus on one side and in the bag on the opposite side. If this is the case, the haptics in the bag may be released and placed in the sulcus. If the haptics are damaged and the capsulorhexis does not allow optic capture, the damaged IOL may be replaced with another sulcus-fixated three-piece IOL.

MICHAEL D. GREENWOOD, MD
Based on the normal examination findings, including topography and tear film, I suspect that the cause of decreased vision is the IOL. In the Figure, slight decentration is evident, but, more important, there is misalignment of the Purkinje images, signaling IOL tilt. This tilting results in internal astigmatism and decreases visual acuity, so repositioning or replacement of the IOL is required.
In cases similar to this one, I find it important to have a backup plan. My approach would be first to ensure that no vitreous is presenting into the anterior chamber and displacing the IOL. I would then try to use the existing anterior capsulotomy to capture the IOL optic. Doing so would allow centering of the IOL and eliminate tilt. One could also try using the posterior capsule, but this is unlikely to be helpful here because of the posterior capsular tear.
If optic capture is not possible because capsular support is lacking, an alternative approach to IOL fixation is required. Options include iris fixation and scleral fixation. My current preference is to use the Yamane technique. Any three-piece IOL may be used, but I prefer the CT Lucia 602 (Carl Zeiss Meditec) because the flexibility of the haptic material facilitates better centration and less tilt. The existing IOL would therefore be exchanged for a CT Lucia 602. After the patient heals from this procedure and the refraction stabilizes, laser vision correction may be required to achieve the desired UCVA.

ALANNA NATTIS, DO, FAAO
The decentered three-piece IOL in the sulcus is likely contributing to this patient’s visual aberrations and dysphotopsias, despite additional refractive treatment. The first step is to obtain excellent visualization of the eye, with particular attention to the integrity of the capsular bag, the anterior capsule, and the presence or absence of prolapsed vitreous, because these findings will influence the treatment approach.
A detailed discussion with the patient is required to ensure she understands that her visual aberrations are probably due to decentration of the IOL and that a secondary intraocular surgery is likely necessary to fix the problem. Because of the complexity and variable outcomes of repairing and replacing dislocated IOLs, all potential operative outcomes should be explained in detail, including a possible future need for surgery as well as retinal precautions in light of the history of high myopia. A backup surgical plan or two are often required to ensure the best possible outcome.
If the IOL is located in the ciliary sulcus and entangled with vitreous, an anterior vitrectomy is required at the very least because the vitreous may be pulling the IOL in one direction or another. Releasing vitreous traction on the IOL sometimes allows recentration without further treatment.
After addressing the vitreous, if anterior capsular support is adequate, the three-piece IOL may be sutured to the iris using a Sinskey or McCannel technique. Given the prior presence of a phakic IOL, before performing iris fixation it would be extremely important to ensure that there are no iris transillumination defects, traumatic mydriasis, or issues with the pupillary sphincter because these can make this surgical technique difficult if not impossible to execute.
If anterior capsular support is lacking and/or iris suture fixation is not an option, it may be possible to combine a glued IOL or Yamane technique with a pars plana vitrectomy. Care must be taken with the haptics of the original IOL because they may not be ideal for scleral fixation (but may be used with caution).
An advantage in this case is that the power of the current IOL is correct. In the worst-case scenario—no capsular support and an inability to fixate the original IOL to the iris or sclera—the options are to exchange the IOL for one that is better suited for scleral fixation or an anterior chamber IOL.

WHAT I DID: ALLON BARSAM, MD, MA, FRCOPHTH
After obtaining informed consent, I performed an IOL exchange using the Sulcoflex (Rayner) as the primary lens. Although this lens is designed as a secondary supplementary IOL, I have used it successfully in similar situations several times when the required power was less than +10.00 D, which is the case for most patients with high myopia. The increased length of the IOL makes it well suited for sulcus fixation. This patient’s high myopia (which necessitated an Artisan lens in the first place) was predominantly axial in nature, and, in my experience, three-piece IOLs do not always center well in the sulcus if optic capture is not possible.
Postoperatively, UCVA was 6/6, and the dysphotopsias totally subsided.