
Most eyes with pseudoexfoliation (PXF) syndrome have open-angle glaucoma, but approximately 9% to 18% have occludable angles that sometimes lead to an acute angle-closure attack.1 The latter situation may occur when zonular laxity causes anterior displacement of the lens-iris diaphragm and secondary angle closure (Figure 1). The video of cataract surgery on an eye with PXF (see video below) is the inspiration for my timeless tips.
SEVEN TIPS
No. 1: Anticipate zonular weakness. Biometry was performed to measure the anterior chamber depth. Eyes with PXF may have a shallow anterior chamber despite a normal axial length, as was the case here (Figure 2). In this situation, I anticipated generalized zonular laxity and ensured that capsular hooks were available on the surgical tray. Zonular laxity in the eye was confirmed intraoperatively by the appearance of striae on the anterior capsule as it was punctured by Utrata forceps (Figure 3).
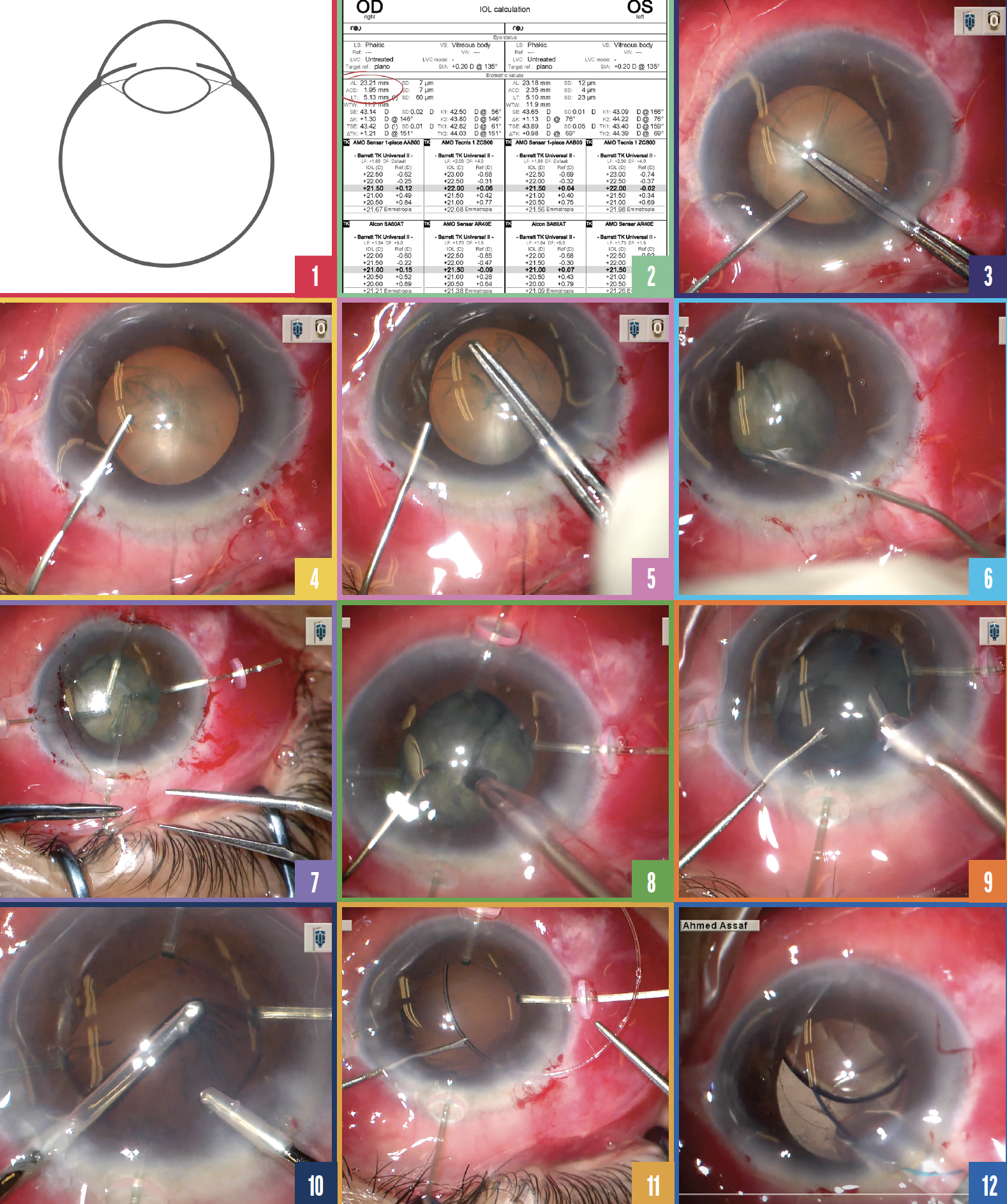
Figure 1. Zonular laxity in eyes with PXF can cause anterior displacement of the lens-iris diaphragm and secondary angle closure.
Figure 2. Zonular laxity should be anticipated if the anterior chamber is shallow but the axial length is normal.
Figure 3. The formation of striae as the anterior capsule is punctured confirms zonular laxity.
Figure 4. An OVD is reinjected periodically to increase tension on the anterior capsule and facilitate the capsulorhexis.
Figure 5. The capsulorhexis is created.
Figure 6. A lack of zonular traction makes rotation difficult after hydrodissection.
Figure 7. Four hooks are placed to hold the lens capsule in the vertical axis during phacoemulsification.
Figure 8. A Neuhann vertical chopper is used to divide the nucleus in half.
Figure 9. The phaco tip is turned sideways during emulsification of the last nuclear fragment.
Figure 10. A swiping movement is made with the I/A handpiece to engage the cortical fibers.
Figure 11. A CTR is inserted before the IOL is implanted.
Figure 12. The plunger is retracted to engage the trailing IOL haptic and push it farther into the anterior chamber.
An OVD was reinjected as necessary to increase tension on the anterior capsule and facilitate the capsulorhexis (Figure 4). In my experience, a capsulorhexis of 5 to 5.5 mm in diameter is ideal in eyes with PXF (Figure 5). Too small an opening can lead to capsular phimosis and shrinkage over time, exacerbating zonular weakness. Too large an opening may not permit safe implantation of a three-piece IOL in the sulcus, if necessary.
No. 2: Stabilize the lens capsule. After hydrodissection, rotation of the nucleus was difficult because of a lack of zonular traction (Figure 6). Four capsular hooks were placed to hold the lens capsule in the vertical axis during phacoemulsification (Figure 7). I favor the Chang modification of MST capsule retractors (MicroSurgical Technology) for PXF eyes. The length of the hooks is reduced, making them easier to insert and helping avoid entanglement of the ends with a capsular tension ring (CTR) at the lens fornix. After placement of the capsular retractors in the case presented in the video, mechanical rotation of the nucleus became possible.
No. 3: Use vertical chopping. I prefer phaco chop techniques that minimize stress on weak zonules. The center of the nucleus was impaled by the phaco tip under high vacuum and low ultrasound power. A Neuhann vertical chopper (Geuder) was used to divide the nucleus in half (Figure 8). The capsular hooks allowed the nucleus to be rotated and divided into smaller fragments without the need to move the chopper to the lens equator behind the iris, as in horizontal chopping. I find this technique works well for eyes with small pupils.
Nuclear fragments were brought to the phaco tip, which was positioned in the center of the chamber. During emulsification of the last quadrant, the phaco tip was turned sideways to reduce the dispersion of ultrasound energy toward the corneal endothelium. Turning the bevel down would have increased the risk of accidentally aspirating the capsule because of the lax zonules (Figure 9).
No. 4: Peel cortex tangentially. Tangential peeling puts much less stress on the zonules than radial peeling. In the video, cortical fibers were engaged with a swiping movement of the I/A handpiece before it was pulled toward the center (Figure 10). Unlike a CTR, capsular hooks do not hold many of the fibers.
No. 5: Delay insertion of a CTR. A CTR is an equatorial stabilizing device that may improve the long-term stability of the capsular bag. Filling the capsular bag with a cohesive OVD before placing the CTR helps protect the zonules.
A CTR was inserted just before IOL implantation (Figure 11). A second instrument was used to position the CTR.
No. 6: Place the IOL in the sulcus. The capsular hooks were removed. An OVD was injected to create space between the iris and anterior lens capsule, and the leading haptic of a three-piece IOL was slowly introduced into the sulcus. Slow pronation movement of the hand guided the unfolding of the IOL. The plunger was retracted to engage the trailing haptic and push it farther into the anterior chamber (Figure 12). With the second instrument, the lens was centered and rotated to bring the trailing haptic into the sulcus.
No. 7: Achieve optic capture. The optic was captured by pressing the sides of the haptic 90º away from the haptic-optic junction. This technique allowed the lens optic to be placed in the bag while the haptics were in the sulcus. Optic capture can prevent pigment dispersion from iris chafing and reduce the risk of early dislocation of the IOL–capsular bag complex.2
CONCLUSION OF THE CASE
The OVD was removed from the anterior chamber and behind the IOL optic. Centration of the IOL was confirmed, and stromal hydration was performed.
1. Patel AS, Salim S, Aref AA, et al. Pseudoexfoliative glaucoma. Eyewiki. July 10, 2022. Accessed December 21, 2022. https://eyewiki.aao.org/Pseudoexfoliative_Glaucoma
2. Chang DF. Stepwise IOL fixation strategies for varying severity of zonulopathy. (2019). In: Chang DF (ed). Advanced IOL Fixation Techniques: Strategies for Compromised or Missing Capsular Support; Slack.



