The evolution of AI and big data has created new paradigms in ophthalmology. Their integration in ophthalmology holds promise for more accurate diagnoses, advances in ophthalmological research, better treatment outcomes, and even improved patient experiences. Big data can also be used in the quest to track patient-reported outcome measures (PROMs), and AI can be used to analyze and interpret the results.
BACKGROUND
Clinical measurements such as visual acuity testing encompass only part of the patient experience and postoperative outcomes. They do not address the impact a disease can have on patients' quality of life (QOL).1 Visual acuity testing remains a core part of the everyday assessment of lens performance. It has also been suggested, however, that clinicians should more closely assess patients' functional vision.2 Functional vision data collection can be achieved with PROMs, which encompass the subjective measurements of patients' perceptions of their health, symptoms, experience, and QOL.
Accurately gathering PROMs plays a crucial role in the shift toward customized and value-based patient care and in understanding how specific treatments affect patients’ lives.3 Additionally, PROM collection helps clinicians address the patient perspective in customized care and inform decision-making, helps practices track clinical performance, and helps staff produce patient-facing educational material. PROMs data can also be used for auditing and revalidation purposes.
The concept of QOL entered health care in the late 1960s.4 Around that time, instruments were developed to determine subjective measures for results that extend beyond medical outcomes, such as psychological well-being, social function, and physical symptoms. In the '80s, many practices started using standardized questionnaires to assess the effect of medical conditions and treatments on various aspects of patients’ lives.5 Throughout the '90s and 2000s, PROMs were refined, and various measurement tools were proposed and incorporated into pre- and postoperative clinical assessments.6 The collection of PROMs, however, has largely been confined to clinical trials owing to the amount of time they take to administer and staffing pressures outside of controlled environments.
One of the more common issues for clinics is the underwhelming response rate that some online PROM systems produce.7 Research suggests that effective PROM software should incorporate human-centered design (HCD).8
HCD is an approach to the design of products, services, and other interactive systems that prioritizes the needs, preferences, and behaviors of users. Many software platforms assume there is a single end user and a single aim, whereas HCD encourages a more holistic approach. The goal of HCD is to create solutions that go beyond function and efficiency by applying human factors to create an intuitive and enjoyable platform that aligns with the user’s values and experiences.
One PROM platform that incorporates an HCD approach is RayPRO (Rayner; see below for a related video), an online cloud-based platform designed to collect clinically validated PROMs after cataract surgery. RayPRO, powered by real-time, long-term patient feedback gathered autonomously via email, can be used to track patients’ long-term visual recovery for 3 years after cataract surgery. The platform acknowledges that there are requirements from multiple different users—administrative staff to upload the data, patients to respond to the questions, and surgeons to interrogate the data to inform their clinic conversations and decisions.
A novel multiple–HCD-designed patient upload function allows administrative staff to upload patient profiles to RayPRO quickly with a drag-and-drop function. Only three pieces of data are required to track PROMs—the patient's email address, date of surgery, and IOL make/model. This requires less input and can reduce resistance from an already stretched administrative staff.
A second advantage to using an HCD PROM system like RayPRO is that it can help establish true lens performance. For example, RayPRO’s latest version provides a comparison view that allows the user to segment individual IOLs and compare their performance both over the long term (3 years) and in real time. The platform design recognizes that comparative data on all IOL makes and models are key. As a result, RayPRO allows users to add data from other manufacturers.
HCD ELEMENTS
In addition to PROM systems, HCD has a variety of other applications in digital ophthalmology that can be used to help overcome the challenges of health care systems. Here, design is a broad term that refers to both the process of designing a system and the outcome of that process. When applied to health care, design can extend to considering common comorbidities for patients that could affect adoption of the innovation.
To design an HCD system in the age of digital ophthalmology, several elements must be considered.
No. 1: User research. An understanding of the needs, challenges, and behaviors of patients should be obtained through interviews, surveys, and observations. Insights into how they feel HCD digital ophthalmology solutions can best support their needs are gathered.
No. 2: User personas. Detailed personas for patients with different eye conditions, ophthalmologists, optometrists, and other eye care providers can be developed to ensure the HCD solutions are tailored to users’ specific needs.
No. 3: Iterative design. An iterative design process involves continuous testing and refinement of prototypes based on user feedback. This helps the digital ophthalmology solution evolve to meet user needs and preferences.
No. 4: Accessibility and inclusivity. HCD digital ophthalmology solutions should be accessible to users with varying levels of visual impairment. It is important to consider incorporating adjustable font sizes, high contrast modes, and compatibility with screen readers to ensure inclusivity.
No. 5: User interface design. The user interface should be intuitive. It should also be clear and simple to navigate with consistent layouts and well-organized content.
No. 6: Data security and privacy. All data should be encrypted, stored securely, and compliant with relevant regulations such as General Data Protection Regulation in the European Union and United Kingdom and HIPAA in the United States.
No. 7: Education and empowerment. Educational elements can be incorporated into digital ophthalmology solutions to help patients understand eye health conditions, treatment options, and best practices. HCD solutions help enhance user engagement and compliance.
No. 8: Feedback channels. Effective HCD systems include clear channels for users to provide feedback, report issues, and suggest improvements. This user-generated input can drive ongoing enhancements of the system's design.
No. 9: Remote monitoring and telemedicine. These technologies boomed during the COVID-19 pandemic. Digital technologies that enable remote monitoring of eye conditions and provide telemedicine capabilities can be especially valuable for patients who have difficulty traveling to health care facilities.
CONCLUSION
Applying HCD principles to digital ophthalmology solutions and the adoption of tools that display big data can help create technologies that are not only advanced but also user-centric (Figure). These solutions have the potential to improve patient outcomes, enhance the patient experience, improve the efficiency of eye care delivery, and contribute to advances in the field.
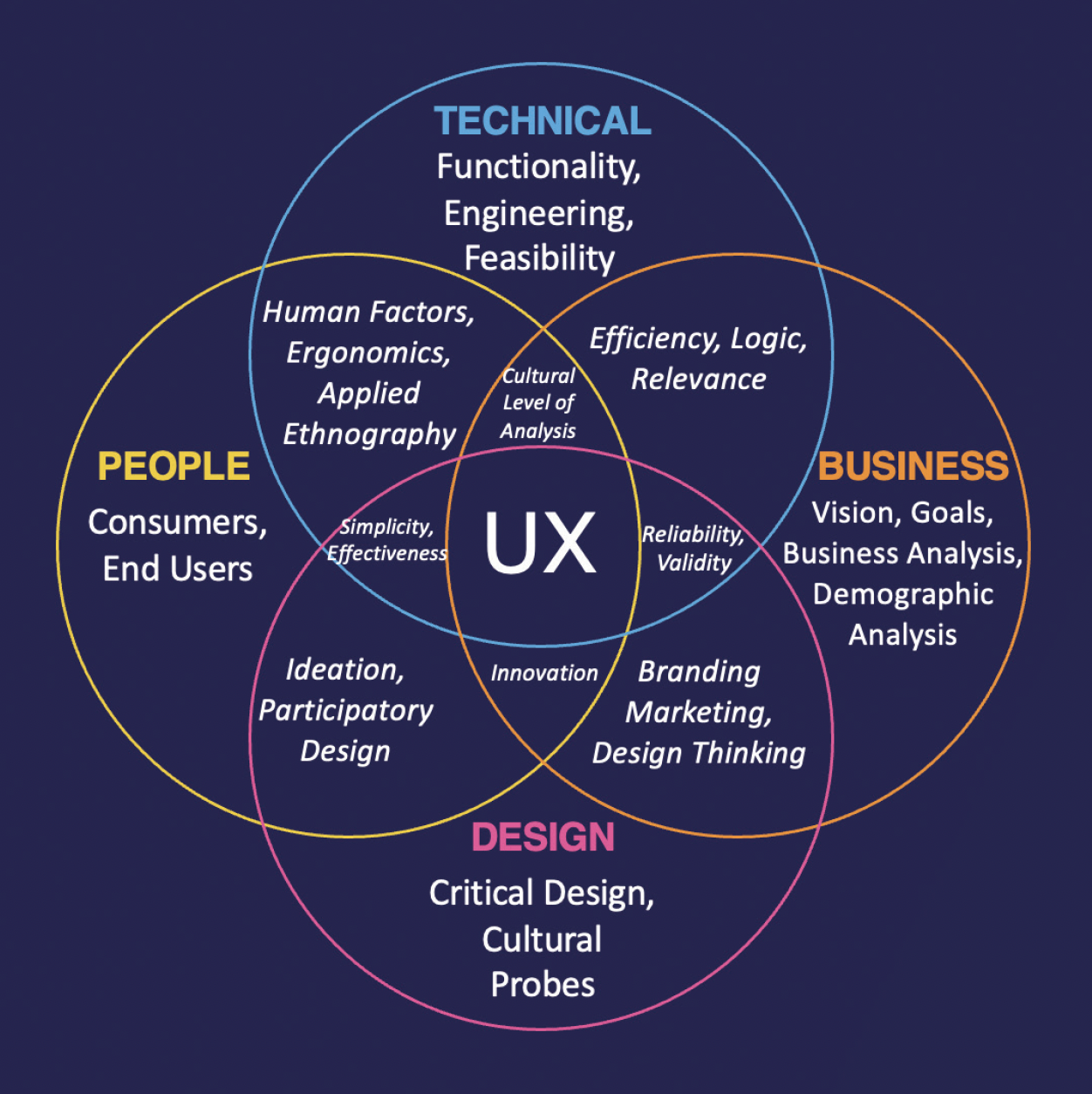
Figure. HCD focuses on creating a user-centric experience.
1. Denniston A, Kyte D, Burr J. An introduction to patient-reported outcome measures in ophthalmic research. Eye. 2014;637-645.
2. Barrett G, Riberiro F, Findl O, Keo, T. Extending range of vision with advanced technology IOLs. Presented at: Asia-Pacific Association of Cataract and Refractive Surgeons; June 8-10, 2023; Singapore.
3. Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Academic Medicine. 2020;95:682-685.
4. Elkington JR. Medicine and quality of life. Ann Intern Med. 1966;64:711-714.
5. Midena D, Yeo R. Toward a history of the questionnaire. Intellectual History Review. 2022;32:503-529.
6. Field J, Holmes M, Newell D. PROMs data: Can it be used to make decisions for individual patients? A narrative review. Patient Relat Outcome Meas. 2019;233-241.
7. Aiyegbusi OL, Roydhouse J, Rivera SC, et al. Key considerations to reduce or address respondent burden in patient-reported outcome (PRO) data collection. Nat Commun. 2022;13:6026.
8. Göttgens I, Oertelt-Prigione S. The application of human-centered design approaches in health research and innovation: a narrative review of current practices. JMIR Mhealth Uhealth. 2021;9(12):e28102.