
Ophthalmologists are no strangers to digital technology, especially given our long-standing use of imaging technologies such as OCT, biometry, and topography. In the past decade, countless advances in digital tools and techniques have improved our ability to diagnose eye conditions and communicate with patients, increased our surgical efficiency and workflow, and even allowed us to deliver care remotely. Digitalization is revolutionizing the way we practice and transforming the health care landscape.
THE PROMISE OF BIG DATA
Big data is defined by three Vs: volume, variety, and velocity.1,2 It has the potential to simplify how we diagnose, treat, and prevent eye disease. In health care, big data is used primarily to analyze large datasets generated from electronic health records (EHRs) and clinical trials. It can be used to identify patterns and risk factors for diseases and assess treatment outcomes. It can also help with the development of predictive models for eye conditions to facilitate early detection and customize treatment plans.
The AAO’s Intelligent Research in Sight (IRIS) Registry is a great example of how big data is being used in ophthalmology. The centralized data repository and reporting tool is used to identify trends and improve patient care. It compiles information from the EHRs of participating ophthalmology practices, which represent about 95% of practices in the United States (Figure).3 The types of data included in the IRIS Registry are listed in the accompanying sidebar.
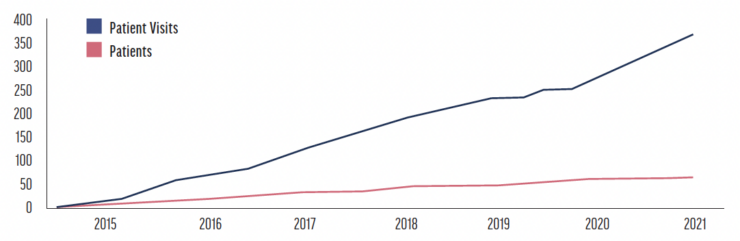
Figure. IRIS registry growth from 2015 to 2021 in millions of patient visits and unique patients.
IRIS Registry: Included Categories
- Vision problems and blindness/Diagnosed vision disorders
- Vision care services/Eye exams
- Vision care services/Imaging or diagnostic tests
- Vision care services/Screening services
- Vision care services/Glasses or contacts
- Age-related macular degeneration/AMD prevalence
- Age-related macular degeneration/AMD treatment
- Cataract/Cataract prevalence
- Cataract/Cataract treatment
- Diabetic retinopathy/DR prevalence
- Diabetic retinopathy/DR treatment
- Glaucoma/Glaucoma prevalence
- Glaucoma/Glaucoma treatment
- Other eye disorders/Prevalence
Abbreviations: AMD, age-related macular degeneration; DR, diabetic retinopathy
Another example is ESCRS’s European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO) Project. Established about 20 years ago, EUREQUO includes data from more than 3 million surgeries. Its main functions are to improve treatment and standards of care for both cataract and refractive surgery, influence the exchange of best practices to improve patient safety, develop evidence-based guidelines for European cataract and refractive surgeons, and foster benchmarking and clinical improvement.4 The EUREQUO database is publicly available to researchers.
IMPROVING PATIENT CARE
Integrating digitalization can improve patient care. First, it has increased the power of virtual communication, whether that be through teleophthalmology or obtaining a second opinion from colleagues around the world. Second, virtual reality (VR) opens a new avenue for surgeon training and education.
Virtual communication. The rise of teleophthalmology ushered in a new era of patient care. Now, patients can receive specialized care remotely in the form of preoperative education and counseling, basic eye examinations, and even general postoperative follow-up. Teleophthalmology allows patients to transmit images and videos of their eyes securely and ophthalmologists to review them virtually. This reduces the need for in-person visits for minor eye issues. Teleophthalmology also expands access to care. Patients who live far from eye care facilities and specialists can undergo basic screenings and follow-up care without leaving their homes. (For more on teleophthalmology, read the article “Transforming Ophthalmology”)
Digitalization also fosters collaboration among eye care professionals. We can consult on difficult cases with colleagues from around the world. Their advice can help with treatment decisions and management tactics and improve postoperative outcomes.
Surgeon training and education. VR platforms can be used to teach surgeons how to treat various eye conditions and practice intricate surgical procedures before entering a human eye. VR can also be used to replicate complex cases, helping surgeons gain confidence and refine their skills in a controlled environment.
DIAGNOSTICS AND SELF-MONITORING DEVICES
Digital ophthalmology can offer a more accurate and efficient way to screen for and diagnose ocular conditions. With the help of big data, deep learning, and AI algorithms, the classification of images and high-dimensional data has gotten more precise. This may allow us to intervene at the earliest signs of disease, reducing the burden on patients and preventing serious vision loss.
Wearable devices that monitor and analyze eye health can support these efforts. Contact lenses have been developed to measure IOP, detect early signs of glaucoma, and track changes in visual acuity. Data collected from wearable devices can help us customize treatment plans, enhancing the patient experience and possibly improving outcomes.
CHALLENGES
No. 1: Data sharing across platforms is not always possible. We ophthalmologists have many different devices that take all kinds of images and produce digital data, but many of them do not work together. The result is that certain data are not transferrable to another platform or device.
No. 2: Harmonization is lagging. To make the most of digitalization, the format of data derived from like devices must be standardized. If all biometry, OCT, and topography devices provided the same output, we could import the data from any machine into standardized formulas and EHRs. This, however, would require manufacturers to come together to define the standards for all core data.
No. 3: The pace of adoption varies. Several barriers affect the adoption of digital ophthalmology, including access to technology and type of practice. Hospitals, which is where I practice, can be slow to transition to a new technology such as EHRs because it requires collaboration between many different specialty clinics and personnel, an IT department, and a project management team. Conversely, ophthalmologists in the private sector can adopt EHRs much earlier because fewer stakeholders are involved and the transition can be more efficient.
No. 4: Data protection. Ethical considerations with digital health care are coming to light. The topic of data protection is beyond the scope of this article and is covered in more detail in the article “Data Are the New Oil.”
THE FUTURE
The way I see it, digitalization promotes reliable, safe, efficient, and customized patient care. It can get patients more involved in their care and increase the level of meaningful engagement we have with them. Digital informational brochures, electronic informed consent, and postoperative questionnaires were only the start. Improvements in EHR software, diagnostic technology, virtual communication, and surgical training and access to large datasets are unleashing the power of digital ophthalmology to improve eye care.
1. Mooney SJ, Westreich DJ, El-Sayed AM. Commentary. Epidemiology. 2015;26:390-394.
2. Price WN, Nicholson Price W, Glenn Cohen I. Privacy in the age of medical big data. Nat Med. 2019;25:37-43.
3. IRIS Registry at a Glance. Centers for Disease Control and Prevention. Accessed May 17, 2023. https://www.cdc.gov/visionhealth/vehss/data/ehr-registries/iris.html
4. The EUREQUO project. European Society of Cataract and Refractive Surgery. Accessed May 17, 2023. https://www.escrs.org/about-escrs/registries/eurequo/


