As a refractive surgeon, I try to consistently implement new technologies to fine-tune and improve the results achieved in cataract and refractive surgery. In my practice, outcomes are monitored, and, over the years—with the advent of femtosecond lasers, new intraocular implants, and image guidance systems—we have made it a priority to achieve better results and greater patient satisfaction. This article provides a brief overview of our recent implementation of selected technologies and how they have improved our outcomes to date.
AT A GLANCE
• The accuracy of cataract and refractive surgery results is high.
• Knowledge of new diagnostic and surgical equipment, the wide variety of IOLs available, and evolving surgical procedures is helping surgeons to fine-tune their outcomes.
• Consistently working to improve surgical outcomes and implementing the technologies necessary to do so can yield greater patient satisfaction and better quality of vision.
LASER-ASSISTED CATARACT SURGERY
My practice introduced the LenSx femtosecond laser and Cataract Refractive Suite (both by Alcon) in 2014. As our experience with these technologies has broadened, it has become easier to highlight how they have affected our results.
Because our practice is oriented to refractive surgery, we see a lot of patients with high ametropias (myopia, hyperopia, astigmatism). These difficult eyes present challenges even for experienced surgeons. In hyperopic patients with shallow anterior chambers or myopic patients with extremely deep anterior chambers, the femtosecond laser carries the advantage of making a more precise and round capsulorrhexis,1 without risk of endothelial touch or slippage of the capsulorrhexis due to difficult maneuverability with forceps in these risky eyes. The laser capsulorrhexis increases the chance of correct positioning of the IOL with complete overlap of the rhexis.2
Softening of the lens with the femtosecond laser makes it possible to reduce phaco energy3 and intraocular rotation of the lens. Due to the preoperative softening and division of the lens nucleus, only minimal rotation of the nucleus intraoperatively is necessary. The gas bubbles produced by the laser provide a kind of pneumatic lens dissection, making the nucleus more mobile inside the capsular bag.
An additional advantage of laser lens division is that hydrodissection can be performed less vigorously. A cannula is placed inside a groove made by the laser, and the mobility of the nucleus is checked without rotation. Nuclear grooves created by the femtosecond laser can be easily cracked without nuclear rotation. The nuclear fragments can be aspirated with minimal or no phaco energy and minimal rotation of the lens. This results in less stress on the zonules, which is beneficial especially in complicated eyes, such as those with loose zonules, subluxated lenses, and pseudoexfoliation. Minimizing the use of phaco energy and maneuvers inside the eye results in a more immediately clear cornea postoperatively and more rapid visual recovery.4 The use of less phaco energy may also be of benefit in eyes with endothelial dystrophies or eyes at risk of inflammation.
Patient flow with laser-assisted cataract surgery must be optimized. In our clinic, the patient enters the OR on the surgical bed and is immediately placed under the LenSx laser. Once the laser portion is complete, the patient bed is moved under the microscope and the eye is prepped with povidone-iodine. Surgery then proceeds in the usual way. Having passed the learning curve, the total procedure now adds only 5 minutes to our conventional phacoemulsification surgery time (Figure 1).
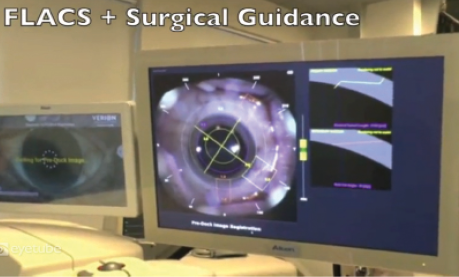
New imaging systems, such as the Verion (Alcon), make it possible to place incisions on the exact desired axis and have more control of surgically induced astigmatism. In patients with low astigmatism, we previously created limbal relaxing incisions or opposite clear corneal incisions. Arcuate keratotomy with the femtosecond laser in combination with the Verion imaging system is more precise and less invasive than manual corneal incisions. This approach also accounts for cyclotorsion by comparing a preoperative image of the eye in an upright position with an image of the eye when the patient is on the operating table. It can reduce even low degrees of astigmatism, which is of particular importance in patients receiving multifocal IOLs (Figure 2).5
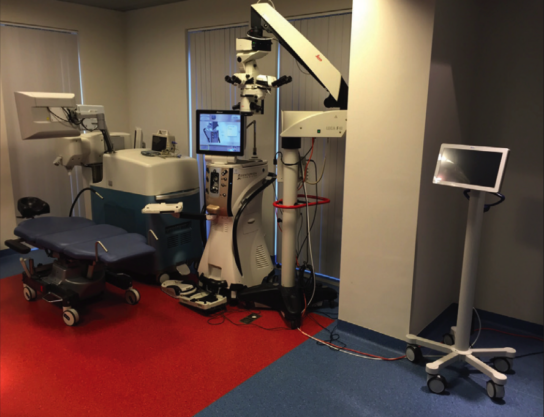
Figure 1. Setup of patient bed, femtosecond laser, phaco machine, microscope, and Verion imaging system.
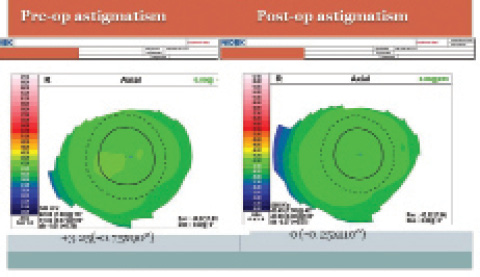
Figure 2. Arcuate incisions with the LenSx laser can be used to reduce even small amounts of astigmatism.
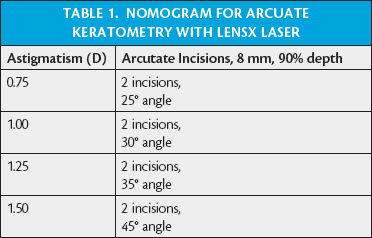
Astigmatism of less than 1.50 D with the rule and 1.00 D against the rule are managed using laser arcuate keratotomy. I set the laser software for 90% depth of OCT-guided corneal pachymetry. No corneal perforations have been observed with this method. We take into account not only the anterior corneal astigmatism but also the posterior cornea by using Scheimpflug technology (Pentacam; Oculus) to calculate the total corneal astigmatism. In the case of against-the-rule astigmatism, we add 5° more to the incision length on our nomogram (Table 1) if the posterior corneal astigmatism is on the same axis as the anterior astigmatism. Since we started performing laser arcuate incisions for lower degrees of astigmatism, we have noticed less residual postoperative astigmatism, fewer enhancements, and increased patient satisfaction. One concern might be the gradual regression of effect of incisional keratotomies; as of the time of this writing, we have not noticed any regression with femtosecond laser arcuate keratotomies. The technology makes the incisions repeatable, as they can easily be reopened at the slit lamp.
For higher degrees of astigmatism, toric IOLs are used. As the imaging system accounts for cyclorotation, toric IOLs are easily placed on the right axis inside the eye.6 In fact, we perform astigmatic correction with the femtosecond laser or with a toric IOL in 35% of our cataract surgeries.
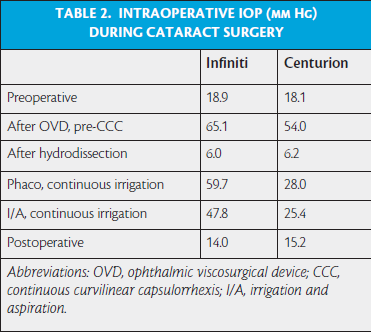
New phaco machines make it possible to have greater control of IOP during surgery. We compared IOP during cataract surgery with two phaco systems: the Centurion Vision System (Alcon), using active fluidics and IOP of 45 mm Hg (n = 20), and the Infiniti Vision System (Alcon), using gravity-based fluidics with a bottle height of 90 cm (n = 20). IOP was measured using three consecutive measurements with the Schiotz tonometer at six points during the cataract operation: (1) preoperatively, (2) after filling the anterior chamber with viscoelastic, (3) after hydrodissection, (4) during irrigation with the phaco probe and (5) irrigation cannula, and (6) at the end of the procedure. Results are shown in Table 2. A remarkable difference in IOP was seen between the two groups with the phaco probe in irrigation mode as well as after the irrigating cannula was placed inside the eye; pressures were lower with the Centurion than the Infiniti at these readings. Having lower and better controlled IOP during the procedure may improve the safety of our surgery, especially in patients with glaucoma.
REFRACTIVE SURGERY
Refractive lens exchange with implantation of a multifocal IOL has grown steadily in volume in our practice over the past few years. The release of new IOLs has broadened our use of presbyopic lens surgery. The trifocal Zeiss AT.Lisa (Carl Zeiss Meditec) and FineVision (PhysIOL) IOLs have focal points at distance, 80 cm, and 40 cm. A new trifocal IOL, Panoptix (Alcon), has focal points at distance, 60 cm, and 40 cm. Other refractive IOLs with high and medium additions (Oculentis) or with enhanced depth of focus (Tecnis Symfony; Abbott Medical Optics) can give patients functional distance, near, and intermediate vision with possibly less glare and fewer halos than multifocal IOLs.
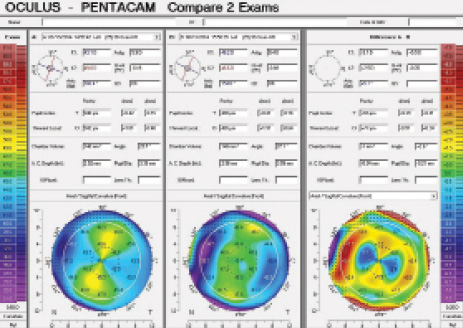
Figure 3. The use of femtosecond LASIK can yield good results in myopia, low hyperopia, and even high amounts of astigmatism.
This range of lens choices enables us to have a better approach to meeting our patients’ lifestyle needs when choosing a multifocal IOL. Working distance may differ for patients using laptop or desktop computers. Reading or working distances may vary depending on the patient’s height. Factors such as occupational activities and lifestyle are important, and all of this must be taken into account when choosing an IOL for a specific patient.
Our refractive outcomes using femtosecond LASIK with the Refractive Suite (Alcon) have shown good results for myopia, low hyperopia, and even high amounts of astigmatism. In 52 consecutive eyes with high astigmatism (2.50 D to 7.00 D; mean, 3.32 D), 94% of eyes were within 1.00 D of target at 3 months postoperative, and there was a 10% chance of gaining lines in BCVA (Figure 3).
Centration of the excimer laser on the apex of the cornea has been improved with the use of preoperative topography (Topolyzer, Alcon), imported into the laser for automatic apex centration. The surgeon still has the ability to decenter the ablation between the pupillary center and corneal apex if desired. In practice, we center the laser between the pupillary center and the corneal apex at a distance of 50%. These centration modalities, along with improved eye tracker quality, contribute to better outcomes postoperatively.7
Another helpful feature is in-line pachymetric readings, which provide a direct calculation of the residual stromal bed.8 This is useful for enhancement procedures, even years after primary LASIK, or if no information on the flap thickness is available.
In an effort to reduce regression of hyperopic LASIK, we use a combination of LASIK with CXL (LASIK Xtra; Avedro).9 In these cases, isotonic riboflavin 0.22% is applied to the stromal bed for 90 seconds with an open corneal flap immediately after excimer ablation. Following this, the corneal bed is rinsed, the flap is replaced, and the UV light treatment is initiated at 30 mW/cm2 for 90 seconds and for a total dose of 2.7 J/cm2.
In our clinic, we implemented the Wavelight EX500 excimer laser (Alcon). In the FDA clinical trials of its precursor (Allegretto EyeQ), 95% of patients with myopia or myopic astigmatism achieved 20/20 and 94% of patients were within ±0.50 D at 3 months postoperative. Because of these results and the immediate postoperative visual rehabilitation, all-laser LASIK is still the preferred procedure in our clinic.
We are, however, looking with great interest at newer refractive surgical techniques such as SMILE. The results of SMILE for myopia and myopic astigmatism vary, with 58% to 96% of eyes reaching 20/20 UCVA and 82% to 100% within ±0.50 D at 3 months postoperative.10-13 Although there seems to be great variability in results, advances in laser technology make this new procedure interesting, and it may gain greater acceptance in the future.
For patients who are not suitable candidates for excimer laser surgery due to high astigmatism or thin or suspicious corneas, we opt to implant phakic IOLs. The advent of the Visian ICL with Centraflow technology (STAAR Surgical) eliminates the need to perform a peripheral iridectomy for this posterior chamber lens. The central opening ensures continuous flow of aqueous, avoiding angle-closure IOP spikes. This shortens the procedure time, reduces surgically induced inflammation, and enhances the results. Due to the central KS-Aquaport—the hole in the optic that allows fluid flow—halos can be recognized in a few patients, although these symptoms seem to be transitory.
CONCLUSION
Today, an expansive range of technologies is available, and results in cataract and refractive surgery are high. Knowledge of new and upcoming diagnostic and surgical equipment, the wide variety of IOLs, and evolving surgical procedures will continue to help us fine-tune our outcomes. In the end, these efforts can benefit our patients and yield greater satisfaction and improved quality of vision.
1. Nagy ZZ, Kranitz K, Takacs AI, Mihaltz K, Kovacs I, Knorz MC. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg. 2011;27:564-569.
2. Kranitz K, Takacs A, Mihaltz K, Kovacs I, Knorz MC, Nagy ZZ. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorrhexis parameters and their effects on intraocular lens centration. J Refract Surg. 2011;27:558-563.
3. Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser-assisted lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refract Surg. 2013;39:1297-1306.
4. Conrad-Hengerer I, Al Juburi M, Schultz T, Hengerer FH, Dick HB. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser-assisted cataract surgery: three-month follow-up. J Cataract Refract Surg. 2013;39:1307-1313.
5. Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323-1329.
6. Elhofi AH, Helaly HA. Comparison between digital and manual marking for toric intraocular lenses: a randomized trial. Medicine (Baltimore). 2015;94(38):e1618.
7. Kanellopoulos AJ, Asimellis G. LASIK ablation centration: an objective digitized assessment and comparison between two generations of an excimer laser. J Refract Surg. 2015;31:164-169.
8. Soeken TA, Apsey DA, Townley JR, Haas RW, Caldwell MC. Comparison of pachymetry measurements between the Alcon Wavelight EX500 and Sonogage Corneo-Gage plus platforms. J Refract Surg. 2015;31:328-332.
9. Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen cross-linking and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013;61:430-432.
10. Pedersen IB, Ivarsen A, Hjortdal J. Three-year results of small incision lenticule extraction for high myopia: refractive outcomes and aberrations. J Refract Surg. 2015;31:719-724.
11. Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism [published online ahead of print November 20, 2015]. Graefes Arch Clin Exp Ophthalmol. doi:10.1007/s00417-015-3226-5.
12. Reinstein DZ, Carp GI, Archer TJ, Gobbe M Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg. 2014;30:812-818.
13. Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of small incision lenticule extraction for the correction of myopia: 1-year follow-up. BMJ Open. 2015;5(11):e008268.
Guy Sallet, MD, FEBOphth
•Practices at the Ooginstituut in Aalst, Belgium
• dr.sallet@ooginstituut.be
• Financial disclosure: Consultant (Alcon)