In cataract surgery, a sufficiently dilated pupil is necessary to allow the surgeon to safely remove the cataract and replace it with an appropriate IOL. When the pupil is not sufficiently dilated, it obstructs the surgeon’s view and makes each step more difficult, increasing the risk of complications during surgery and unfavorable outcomes postoperatively.
These increased risks can be avoided if the pupil is dilated well before starting surgery. This article describes a reversible method that I call the Idrees intracameral pupil-dilating technique and presents the rationale for its use.
AT A GLANCE
- The Idrees intracameral pupil-dilating technique takes advantage of the muscle control of the iris.
- During the technique, 1% preservative-free lidocaine is applied to the entire anterior surface of the iris; the lidocaine causes topical anesthesia to the sphincter of the pupil, and the dilator becomes uninhibited, leading to pupil dilation.
- Injection of carbachol into the anterior chamber at the end of surgery causes the pupil to constrict again.
SURGICAL RISKS WITH SMALL PUPILS
Among the most prominent challenges with a narrow pupil, performing capsulorrhexis or anterior capsulotomy of sufficient diameter is not possible. When a satisfactory opening in the anterior lens capsule cannot be fashioned, subsequent steps become more difficult. For instance, you cannot deliver the lens nucleus or perform phacoemulsification if you do not have a sufficient view to ensure safety.
The chances of accidentally touching the iris with surgical instruments increases markedly, and this can result in a cosmetically disfiguring pupil appearance, sometimes associated with glare. Moreover, chances of damage to the capsular margin are increased due to poor visibility. Emulsification risks damage to the posterior lens capsule, which opens the door to other complications later.
It is difficult to get a sufficient red fundus reflex with a poorly dilating pupil. Implanting the IOL poses its own set of potential complications, such as decentration and subsequent malpositioning of the IOL.
Operating through a small pupil can result in iris bleeding, iris prolapse into the wound, or incomplete evacuation of cortical material. Additionally, iris chafing can contribute to increased postoperative inflammation and iris defects that can create cosmesis concerns.
PUPIL DILATION: MECHANISM AND TECHNIQUE
In order to achieve a satisfactorily dilated pupil in every case, you must have a number of approaches at your disposal; some of the most common techniques are described in Getting the Pupil to Dilate.
Unfortunately, most maneuvers for enlarging the pupil during cataract surgery and preventing intraoperative miosis are not ideal. They can cause increased risks of iris sphincter tear, bleeding, iris damage, and severe postoperative fibrinoid reaction. They also may result in changing the shape of the pupil, especially in patients with pseudoexfoliation syndrome, chronic uveitis, glaucoma, or diabetes.
Pupil size is controlled by two muscles—the dilator, which, when stimulated, causes pupil dilation, and the sphincter muscle, which is responsible for constricting the pupil. The dilator is supplied by the sympathetic nervous system and the sphincter by the parasympathetic nervous system. A delicate balance between these muscles determines the size of the pupil under normal conditions. Any disease affecting the nerve supply or the muscles can cause abnormality in the size and shape of the pupil.
As individuals reach the stage of life at which cataract formation is common, most develop some disease that can affect the pupil. At minimum, age-related changes in the iris can cause the pupil to behave abnormally. If the parasympathetic nerve supply is paralyzed, then the sympathetic nerve system takes over and causes the pupil to dilate, and vice versa.
A UNIQUE APPROACH
My intracameral technique for pupil dilation takes advantage of the muscle control of the iris. Once I enter the anterior chamber, I irrigate 1% preservative-free lidocaine into the chamber, onto the entire anterior surface of the iris. I leave this for about 2 minutes, as I have found that there is a critical relationship between the timing and a satisfactory outcome regarding pupil dilation with this technique.
The lidocaine causes topical anesthesia to the sphincter of the pupil, and the dilator becomes uninhibited, leading to pupil dilation. By leaving the lidocaine in place for 80 to 120 seconds, the anesthetic effect is well established before I proceed to the next step (Figure 1).
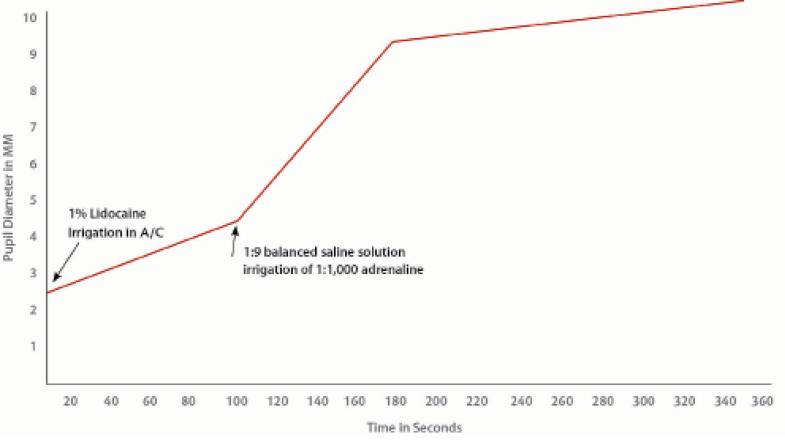
Figure 1. The relationship between the pupil diameter and the time following irrigation of lidocaine followed by dilute adrenaline irrigation.
Once the required time has passed, I irrigate a dilute solution of adrenaline 1:1,000. The dilution is 0.2 mL adrenaline with 0.8 mL balanced saline solution. This stimulates the dilator muscle of the iris, causing further pupil dilation. This takes place in less than 1 minute.
An interesting and useful feature of this intracameral method is that, when carbachol is injected into the anterior chamber at the end of surgery, the pupil responds to this and constricts again (Figure 2). If the carbachol is not irrigated at the end of surgery, the pupil remains well dilated for more than 24 hours and comes back to its normal diameter within 3 days.
If needed, the technique can be repeated during surgery. A 30-gauge cannula mounted on an insulin syringe can be used for intracameral irrigation.
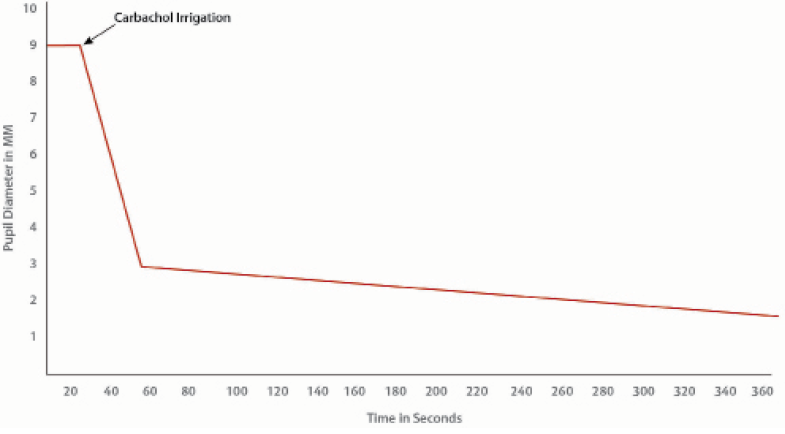
Figure 2. The response and relationship between intracameral irrigation of carbachol and constriction of the pupil at the end of IOL implantation.
ADVANTAGES AND LIMITATIONS
The Idrees intracameral pupil-dilating method is a helpful technique with a valid scientific basis. In my experience, it is safe in patients with no structural pathology in the iris or the muscles that control pupillary diameter. Further, in my experience, it is effective in patients taking medication for enlarged prostate and in those with diabetes, hypertension, or ischemic heart disease.
The greatest advantage of this technique, in my opinion, is that it makes cataract surgery safe. As noted, we cannot safely perform cataract removal through an insufficiently dilated pupil as it affects intraoperative visualization.
My intracameral pupil-dilation technique may not be effective if there are dense posterior synechiae or structural abnormalities (gross or microscopic) of the iris or pupil. However, if synechiolysis is performed before proceeding with this technique, it can work well.
Getting the Pupil to Dilate
Eye Drops
Dilating drops, such as 2.5% phenlyephrine or 1% tropicamide, must be instilled by the patient over some period of time preoperatively. In some cases, due to improper technique on the part of the patient, the effect is not satisfactory, or there may be side effects related to the drops. Topical NSAIDs are also useful to keep the pupil dilated during surgery.
Viscomydriasis
Use of an OVD can produce mechanical dilation. However, the effect is usually not of sufficient duration to allow risk- and stress-free surgery.
Mechanical Devices
A variety of hooks, rings, and retracting devices are available for pupil stretching and dilation. These devices add cost, add insertion and removal time to surgery, provide limited preset dilation for the duration they stay in the eye, and involve risks including permanent change to the shape of the pupil and damage to the corneal endothelium. In eyes with posterior synechiae, these devices have limited potential for use. Examples include the Perfect Pupil (Milvella), Morcher Pupil Dilator, Siepser Iris Protector (EagleVision), and Graether Pupil Expander (EagleVision).
Sphincterotomy
The pupil can be dilated by performing multiple small sphincterotomies along the pupil margin. This approach is quite invasive. It affects the shape of the pupil permanently and can result in an unpleasant cosmetic appearance of the pupil for the rest of the patient’s life.
Intracameral Injection in Irrigation Fluid
Some surgeons add medications to the irrigation solution to dilate the pupil. The effect of this continuous exposure on the corneal endothelium can be harmful, especially in eyes with an already low endothelial count.
Intracameral Injection
Accidental injection of lidocaine into the anterior chamber by an ophthalmologist many years ago suggested the basic concept of intracameral pupil dilation, which is further explained in the main body of this article.
CONCLUSION
Cataract surgery in the presence of a small pupil remains one of the most challenging surgical procedures. Use of a minimally invasive approach to reduce surgical trauma allows the surgeon to effectively minimize the risk of complications and provide patients with the best possible visual and anatomic outcomes.
Each complication arising due to a poorly dilating pupil can be associated with a cascade of subsequent complications, potentially causing unsatisfactory visual outcomes along with mental stress for the operating surgeon and fear of medicolegal proceedings as well.
A well-dilated pupil, by contrast, makes surgery safe, easy, and relatively free from stress for the surgeon. In view of this, cataract surgeons must take all possible steps and measures to ensure that we start with a well-dilated pupil and that the pupil remains dilated throughout the procedure.
Obviously cataract surgery is the most common and most important indication for pupil dilation, but the Idrees intracameral pupil-dilating technique can also be helpful in vitreoretinal surgery, when the surgeon needs a well-dilated pupil for proper intraoperative manipulation. It can also be used to break fresh posterior synechiae in the event of a severe uveitis attack.