
Poor visual acuity affects millions of people worldwide. The condition can be caused by myopia, hyperopia, astigmatism, and higher-order aberrations (HOAs). The last can affect visual acuity and quality of vision even after sphere and cylinder have been corrected. The corneal surface is the source of most HOAs, but some arise from the crystalline lens or, more rarely, the endothelium.
Each optical component of the eye contributes to the refractive index. The tear film, for example, is extremely influential, which means slight irregularities in the anterior corneal surface can degrade visual acuity. Some patients with corneal HOAs achieve a greater improvement in quality of life from their elimination than the correction of their refractive error.
PREOPERATIVE EXAMINATION
Effective customized or wavefront-guided excimer laser treatments can result in better visual outcomes and a lower risk of complications than traditional excimer laser surgery.
The latest diagnostic devices provide quantitative and qualitative analyses of various optical properties, including corneal curvature, elevation, pachymetry, power, and wavefront errors. The most recent advance is the ability to measure the epithelium with anterior segment OCT. Earlier research provided insight into epithelial remodeling after refractive surgery1 that surgeons can take into account when planning laser treatment. It must be remembered, however, that biomechanical weakening and changes in the curvature gradient influence overall corneal shape and can therefore impair vision.2
PLANNING AND TREATMENT
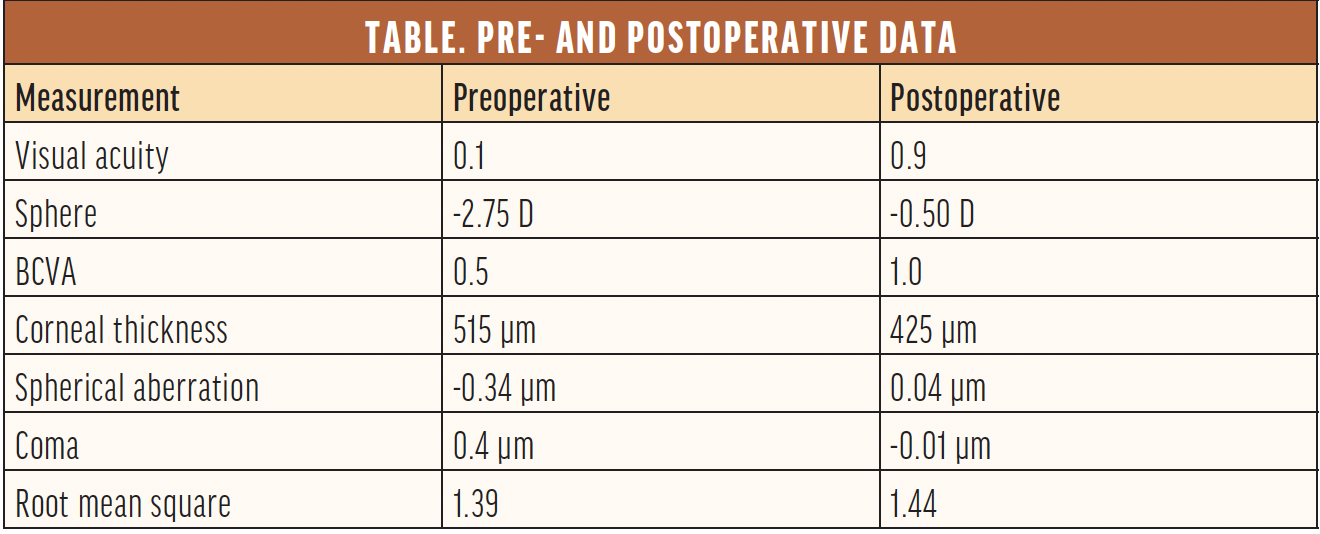
Surgical planning. Customized excimer laser treatment that targets HOAs can improve patients’ visual acuity and overall quality of vision, but it cannot always achieve an emmetropic result (Figure). Corneal thickness, the degree of refractive error, and the overall health of the eye factor into the outcome (Table). Effective surgical planning requires a deep understanding of ablation algorithms and their influence on the optical system.
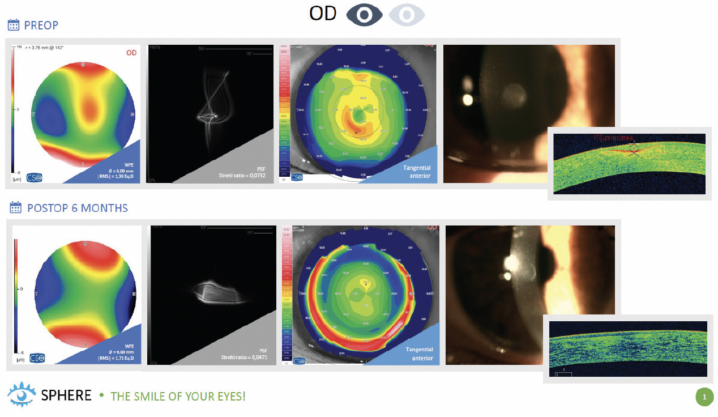
Figure. A customized transepithelial PRK treatment performed for a patient with a corneal scar.
Treatment options. Some excimer laser systems have software that can automatically identify the refraction. This is most beneficial to save corneal tissue instead of simply targeting emmetropia. Whether the planning is done manually or automatically, another key is to determine which HOAs impair the patient’s visual acuity and then target a treatment to eliminate them. This selective approach can save corneal tissue.
▶ Option 1. The STARE-X protocol, developed by Rechichi and Mazzota,3 combines customized removal of the epithelium and HOA treatment with CXL to improve corneal regularity in keratoconic eyes.
▶ Option 2. Shetty described the topography-based removal of the corneal epithelium in keratoconic eyes to improve patients’ vision. Treatment regularizes the cornea, after which accelerated CXL is performed. The ablation depth and area are customized.4
▶ Option 3. Sequential customized therapeutic keratectomy is another tissue-sparing approach that reshapes the corneal surface to address HOAs. Wavefront-guided customized transepithelial ablation that prioritizes the correction of HOAs is performed, followed by wet phototherapeutic keratectomy (PTK).5,6 The idea of regularizing and smoothing the anterior corneal surface with the help of PTK and a masking fluid has been around since the early days of broad beam excimer lasers.7,8
▶ Option 4. PTK alone may be an option for some patients with poor visual acuity due to recurrent corneal erosions, corneal dystrophy, corneal degeneration (eg, climatic droplet keratopathy, Salzmann nodular degeneration, calcific band keratopathy), corneal scarring, bullous keratopathy, keratitis, keratoconus, and possibly refractive surgery complications.9 Other options exist but are not mentioned here.
CONCLUSION
For certain individuals, corneal HOAs have a more deleterious impact on their visual acuity than refractive error. Several customized surgical approaches to eliminating HOAs have been described. The goal of treatment is to enhance patients’ quality of life while conserving corneal tissue.
1. Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness in the normal cornea: three-dimensional display with Artemis very high-frequency digital ultrasound. J Refract Surg. 2008;24(6):571-581.
2. Vinciguerra P, Roberts CJ, Albé E, et al. Corneal curvature gradient map: a new corneal topography map to predict the corneal healing process. J Refract Surg. 2014;30(3):202-207.
3. Rechichi M, Mazzotta C. CXL alone versus in combination with the STARE-X protocol. Cataract & Refractive Surgery Today Europe. October 2018. Accessed June 8, 2023. https://crstodayeurope.com/articles/oct-2018/cxl-alone-versus-in-combination-with-the-stare-x-protocol
4. Shetty R, Ahuja P, D‘Souza S, et al. Simultaneous topography-guided PRK/CXL versus topography-assisted PTK/CXL: 1-year prospective outcomes in keratoconic eyes. J Refract Surg. 2021;37(8):562-569.
5. Vinciguerra P, Lippera M. Sequential customized therapeutic keratectomy. Cataract & Refractive Surgery Today. February 2022. Accessed June 8, 2023. https://crstoday.com/articles/feb-2022/sequential-customized-therapeutic-keratectomy
6. Vinciguerra P, Vinciguerra R, Randleman JB, Torres I, Morenghi E, Camesasca FI. Sequential customized therapeutic keratectomy for Reis-Bücklers’ corneal dystrophy: long-term follow-up. J Refract Surg. 2018;34(10):682-688.
7. Rapuano CJ. Excimer laser phototherapeutic keratectomy. Int Ophthalmol Clin. 1996;36(4):127-136.
8. Sekundo W, Geerling G. Phototherapeutische keratektomie. Grundprinzipien, techniken und indikationen. Ophthalmologe. 2006;103(7):563-569.
9. Deshmukh R, Reddy JC, Rapuano CJ, Vaddavalli PK. Phototherapeutic keratectomy: indications, methods and decision making. Indian J Ophthalmol. 2020;68(12):2856-2866.



