Ahmed Assaf, MD, PhD, FRCS(Ed)
"Social media is an excellent tool for communicating with individuals you wouldn’t otherwise have access to. I often share videos of my cases on Instagram, Facebook, LinkedIn, and YouTube to educate a broader network of my colleagues in ophthalmology. Sometimes, I get bright ideas from folks online for fine-tuning the management technique for similar cases in the future. The following is an example of a case I shared on social media and the responses I received (Figure 1).
Figure 1. The eye on presentation (A). Dr. Assaf’s social media post (B). The responses to Dr. Assaf’s social media post (C).
Figures 1– 12 courtesy of Ahmed Assaf, MD, PhD, FRCS(Ed)
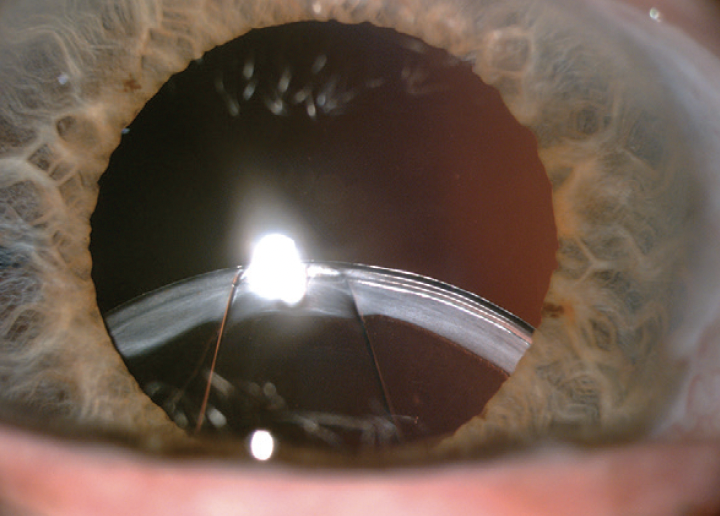
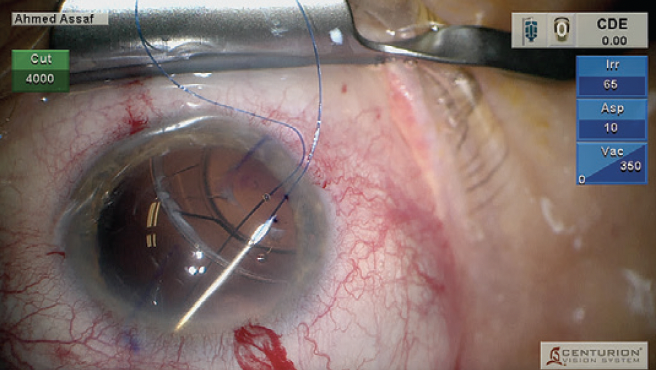
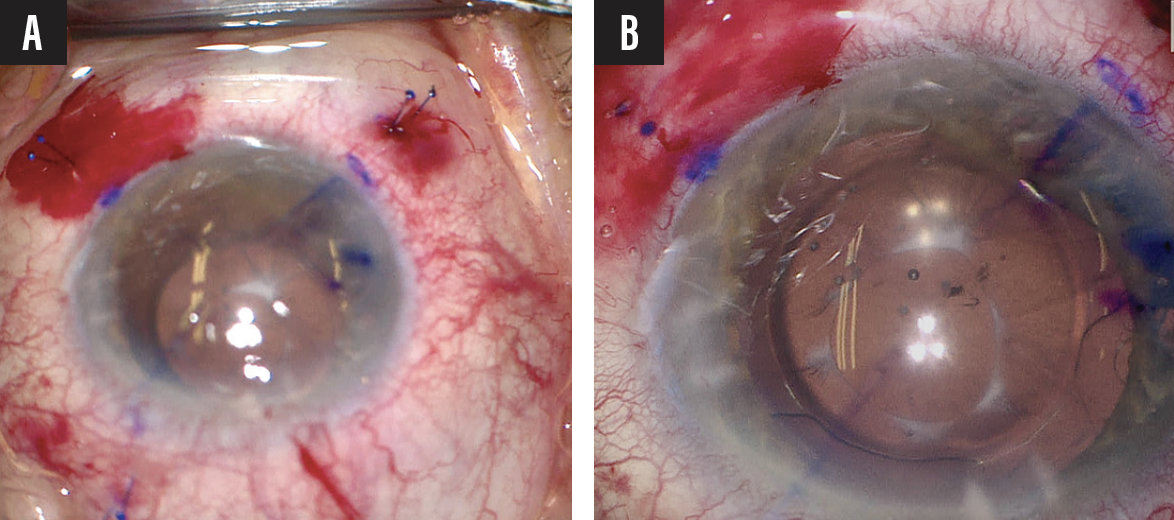
A patient who underwent cataract surgery with capsular tension ring (CTR) implantation at another facility several years ago presented with pseudoexfoliation syndrome in the right eye and a subluxated IOL–capsular bag complex (Figure 2).
Figure 2. Slit-lamp photograph of the right eye showing pseudoexfoliation and a subluxated IOL–capsular bag complex.
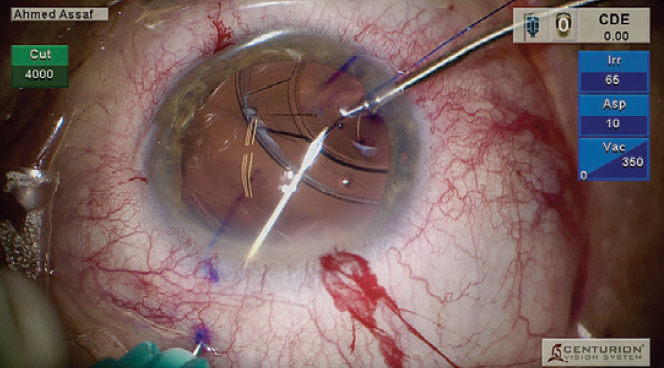
At the beginning of surgery, the lens-bag-CTR complex was massively dislocated; about 270º of zonular loss was observed in the superior quadrant. The plan was to suspend the lens-bag-CTR complex with 6-0 polypropylene sutures (Prolene, Ethicon) in the superior quadrant to center the lens in relation to the pupil.
Figure 3. The first loop is created.
Figure 4. With microforceps, a 6-0 polypropylene suture is threaded through an opposite inferior paracentesis and externalized in the superior quadrant.
Figure 5. The second end of the suture is threaded inside the lumen of a 27-gauge needle 1.5 mm from the limbus.
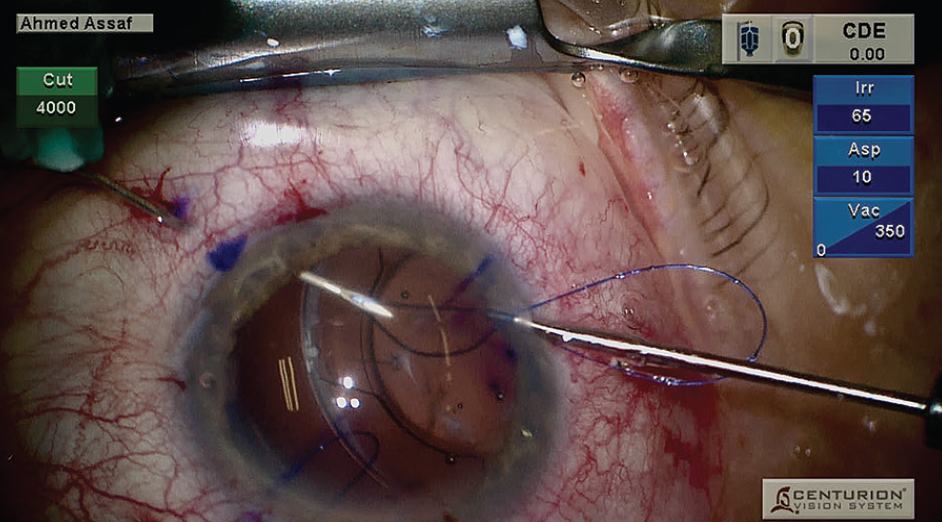
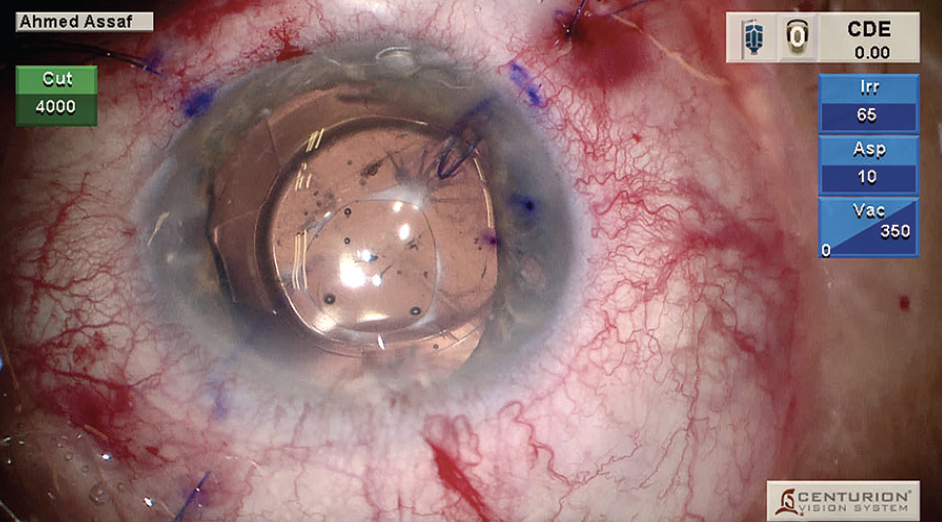
A 27-gauge needle was passed 2.5 mm from the limbus, underneath the CTR, and through the lens capsule to create the first loop (Figure 3). With microforceps, one end of a 6-0 polypropylene suture was threaded through an opposite inferior paracentesis and externalized in the superior quadrant (Figure 4). The second end of the suture was introduced into the anterior chamber and threaded inside the lumen of a 27-gauge needle 1.5 mm from the limbus to form the loop (Figure 5). The needle was withdrawn to externalize the suture on the conjunctival surface. Both ends of the suture were then externalized to form the first loop (Figure 6). A second loop was made in the upper temporal quadrant using the same technique (Figure 7). The two loops were used to suspend the lens-bag-CTR complex (Figure 8). A third loop was made in the inferior quadrant to provide additional support to the complex and minimize the risk of future subluxation due to progressive zonulopathy (Figure 9).
Figure 6. Both ends of the suture are externalized.
Figure 7. A second loop is made in the upper temporal quadrant.
Figure 8. The two loops are used to suspend the IOL–capsular bag–CTR complex.
Figure 9. A third loop is made in the inferior quadrant.
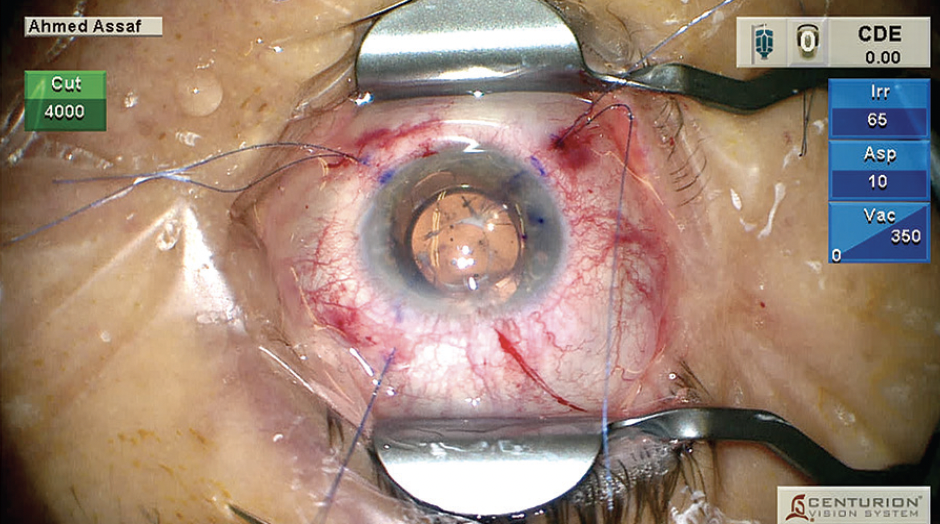
The IOL–capsular bag–CTR complex was recentered by adjusting the tension on each suture loop (Figure 10). The sutures were shortened, and a knob was created at each end with low-temperature cautery (Figure 11A). The IOL was centered with further titration of the tension of each suture loop, and the knobs were buried under the conjunctiva (Figure 11B).
Figure 10. The tension on each suture loop is adjusted to center the IOL–capsular bag–CTR complex.
Figure 11. Knobs are created with low-temperature cautery at the end of each suture and buried under the conjunctiva (A and B).
Postoperatively, the patient’s distance refraction was 0.90 -0.50 D x 150º (Figure 12).”
Figure 12. Postoperative slit-lamp photograph.

J. Morgan Micheletti, MD
"Many of my posts and stories are unique cases that I hope will be of educational value to my physician followers. Most of the time, I’ve already performed the surgery or treatment in the presented cases. As such, I don’t have an example where someone commented or posted advice that I utilized, but I have had numerous fruitful conversations via direct messages that have led to new ways of thinking or generated professional connections. This is, ultimately, where I believe that social media can be highly beneficial: connections.
Social media has been instrumental in allowing me to forge relationships with both industry and surgeons across the world, making it easier to connect with them at meetings. This has led to changes in my surgical approach and thought processes and the introduction of new ideas in my practice.
A word of advice to those looking to start posting videos (be it to Instagram, YouTube, Eyetube, or another social media channel): Steel yourself for comments on ways you ‘should have’ or ‘could have’ done it better. Although most engagements are beneficial and well intentioned, please remember not to feed the trolls. Also remember that posting videos on Instagram, for example, has limitations—for example, I wish my videos and posts were more easily searchable.”

Ben LaHood, MD, MBChB(dist), PGDipOphth(dist), PhD, FRANZCO
"I often post images and videos of interesting cases on my Instagram account (@drbenlahood). Mostly, this is aimed at educating, sharing my experiences (both good and bad), and giving advice about certain anterior segment scenarios. It is a great forum to connect with colleagues and can often be one of the fastest ways to gain advice from around the world. I'm sure that some surgeons would feel that the idea of openly asking for advice about a surgical scenario might make them appear less competent, but my view is that, if it benefits my patient, then I could not care less about my ego.
A recent example of a case where I received great advice from my global colleagues was a large pterygium that had covered the visual axis in a young patient with no ocular comorbidities (Figure 13). In Australia, where I practice, health care is readily accessible, so it is rare to see a pterygium this advanced. I received comments and private messages of advice from surgeons around the world who encounter such severe pterygia much more frequently. The key pieces of advice that helped shape my surgical plan in this situation were as follows:
- Consider using mitomycin C (MMC) at the site of the pterygium excision to help prevent recurrence (from a surgeon in Canada);
- Send the sample for histologic examination (from a surgeon in Morocco);
- Consider using an amniotic membrane to help with corneal defect healing (from a surgeon in India); and
- Postoperatively, consider phototherapeutic keratectomy to normalize the cornea (from a surgeon in Israel).
Figure 13. Preoperative view of a large pterygium covering the visual axis.
Figures 13–15 courtesy of Ben LaHood, MD, MB ChB(dist), PhD, FRANZCO
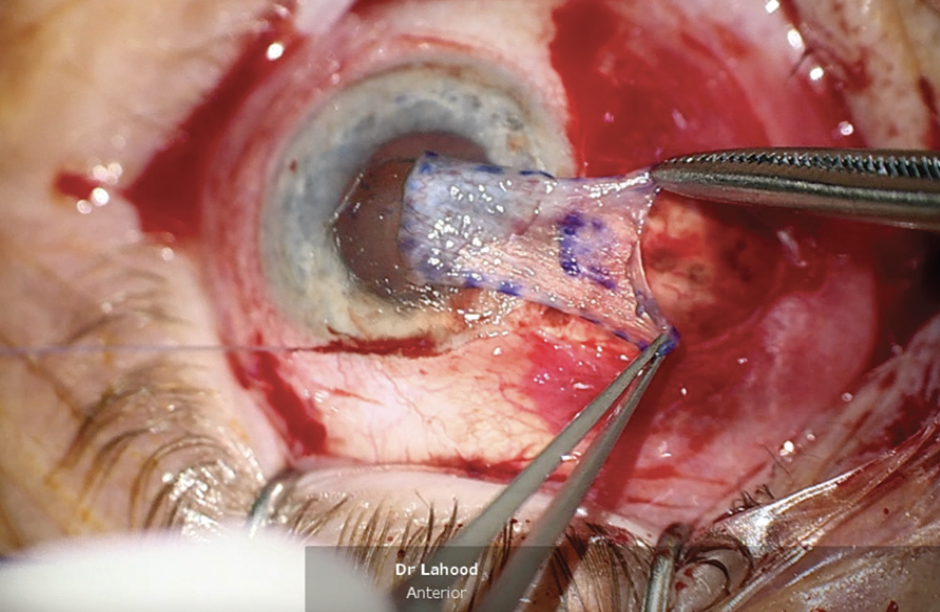
I recently operated on the eye, and I administered MMC at the time of surgery to help prevent a recurrence (Figure 14). I appreciated the idea of using an amniotic membrane for corneal wound healing but decided against it. I determined that I did not need to burden the patient with the additional cost since the eye otherwise looked healthy and had no indications of limbal stem cell deficiency. I sent a sample for histologic examination and will consider phototherapeutic keratectomy to normalize the cornea in the future once it heals and the epithelium remodels (Figure 15).
Figure 14. Conjunctival autograft being applied following the application of MMC.
Figure 15. At the conclusion of the procedure, the conjunctival autograft has been glued in place, and there is a large corneal epithelial defect.
It was great to hear experienced surgeons share their practical pearls, and I will share the results with them soon. Of course, it is vital to have patient consent to share their images and to be wary of those online giving medical advice when you have not met them in person. Finding this kind of expertise either locally or via other means would have been virtually impossible. Social media certainly has a role in disseminating knowledge in ophthalmology."

Mo Ziaei, MBChB(Hons), MD, Cert-LRS, FRCOphth, FRANZCO
"A 57-year-old presented to the ER for reduced vision and irritation 7 days after being hit in the eye with a rose branch while gardening. The patient’s history was notable for myopia correction with LASIK 15 years prior. Initial examination showed a UCVA of 6/6 with a tear in the inferior edge of the flap and some debris under the flap but no corneal infiltrate or ingrowth (Figure 16). The patient was initially treated with topical antibiotics and steroids and was closely observed. Over the course of 2 weeks, the patient developed florid and aggressive epithelial ingrowth, which reduced their UCVA to 6/9 due to irregular astigmatism induction.
Figure 16. Before surgery, there is a tear in the inferior edge of the LASIK flap with significant epithelial ingrowth.
Figures 16 and 17 courtesy of Mo Ziaei, MBChB(Hons), MD, CERT-LRS, FRCOphth, FRANZCO
It was clear that surgical intervention was required for ingrowth removal. I was, however, left with a dilemma of choice of simple ingrowth removal with a high risk of recurrence at the torn edge or removal of ingrowth with adjuvant suturing of the torn edge with a potential risk of inducing irregular astigmatism. After a discussion with local colleagues, I decided to consult the global network of experts that I’m connected with via social media platforms such as LinkedIn and Instagram.
The response was encouraging, with many offering advice based on their prior experience and pearls of wisdom. Most experienced refractive surgeons who responded suggested that I should avoid suturing the flap edge initially and agreed that flap edge approximation, given the degree of tissue loss, would lead to significant irregular astigmatism. Armed with this advice, I proceeded with simple ingrowth removal, application of ethanol, epithelial recession, and bandage contact lens application. The patient did remarkably well, with the resolution of the ingrowth and regaining of a UCVA of 6/6 (Figure 17).”
Figure 17. Postoperatively, the ingrowth has been resolved.