What’s in a Name?
Balamurali Ambati, MD, PhD, and Tanya Trinh, MBBS, FRANZCO
The following line from Shakespeare’s The Tragedy of Romeo and Juliet, “A rose by any other name would smell as sweet,” holds that things remain what they are regardless of what you name them. Words matter, however, and language frames thought. Technical jargon can make doctors seem aloof and repel patients. The use of multiple names for a single procedure can sow confusion, stoke anxiety, erode confidence, and hinder decision making. Using brand names only for a procedure is neither medically appropriate nor professional because it creates an unfair advantage for a single manufacturer.
It is up to us as refractive surgeons and physicians to choose the terms we share with patients. We should not leave the task to manufacturers; it is our responsibility to educate patients and advance the field. The Refractive Surgery Alliance (RSA) Terminology Committee was formed to standardize terminology for the following:
- Replacement of the crystalline lens for the treatment of refractive error and/or presbyopia;
- Lenticule extraction procedures; and
- The phenomenon of transient hyperesthesia with ocular surface issues after any ocular surgery.
One of us (T.T.) led the committee. Additional members included the other of us (B.A.); Dagny Zhu, MD; Lance Kugler, MD; R. Luke Rebenitsch, MD; Guy Kezirian, MD, FACS; Arthur B. Cummings, MMed(Ophth), FCS(SA), FRCSEd; and Brett Mueller, DO, PhD. We solicited the perspectives of the RSA membership (about 500 refractive surgeons worldwide) on terminology for the three areas. The committee met to discuss options and develop recommendations. Our priorities were patient understanding, accuracy, and a brand-neutral perspective. This article shares our recommendations and rationale.*
NO. 1: LENS REPLACEMENT
Lens replacement with an advanced technology IOL is an excellent procedure for patients with presbyopia and cataracts who wish to reduce their dependence on spectacles and contact lenses. The best IOL for each patient is determined by the treating physician.
The committee considered various terms for the procedure, including refractive lens exchange, clear lens exchange, laser lens upgrade, lifestyle lens upgrade, and lens implant focusing enhancement. We decided on lens replacement (LR) because of its simplicity and because patients already understand the concept underlying knee replacement and hip replacement, where a dysfunctional part of the body is removed and replaced to enhance function and lifestyle. The term lens replacement also allows individual physicians to use the words custom, precision, or dysfunctional as a prefix based on their specific needs or context.
NO. 2: LASER-ASSISTED LENTICULE EXTRACTION
Carl Zeiss Meditec launched and trademarked SMILE worldwide. Similar procedures are available in other countries. These include cornea lenticule extraction for advanced refractive correction (CLEAR), performed with the FEMTO LDV laser (Ziemer); femtosecond lenticule extraction (RELEX and FLEX), both performed with the VisuMax laser (Carl Zeiss Meditec); small-incision lenticule keratomileusis (SILK), performed with the Elita Femtosecond Laser (Johnson & Johnson Vision), which the company announced on March 1 received the CE Mark in Europe; and SmartSight, performed with the Atos laser (Schwind eye-tech-solutions).
What all these procedures have in common is the use of a femtosecond laser to create a refractive lenticule inside the cornea that is then extracted. The committee thought that it was crucial to avoid the confusion and anxiety caused by a proliferation of terms for LASIK during its early years. We recognized, moreover, that the German Commission on Refractive Surgery had chosen the term laser lentikle extraktion for this class of procedures in Germany. We also sought opinions from our Spanish- and Portuguese-speaking communities to rationalize the use of the -ex suffix from a cultural context. Laser-assisted lenticule extraction (LALEX) therefore became our term of choice.
NO. 3: SURGICAL TEMPORARY OCULAR DISCOMFORT SYNDROME
Patients can experience ocular discomfort after any eye surgery. The causes are multifactorial and include incision of corneal nerves, toxicity of povidone-iodine or chlorhexidine to corneal epithelial cells or conjunctival goblet cells, inflammation, and preexisting dry eye disease or blepharitis.
The committee’s goal was to come up with a term that validates the discomfort patients experience (they too often feel dismissed by the term dry eye) and emphasizes that, in general, the discomfort decreases over time with healing. We also required that the term acknowledge the inflammatory and nerve components of discomfort that can occur after eye surgery and recognize that it should not be tied to any one procedure. We know that ocular discomfort may also occur as the eye heals after injury or trauma.
We considered several terms: transient innervation dysfunction after eye surgery (TIDES), ocular surgical surface recovery (OSSR), transient induced corneal hyperesthesia (TICH), and laser-associated temporary tear film episode (LATTE). Ultimately, we chose surgical temporary ocular discomfort syndrome (STODS) because it is broader and should be more understandable to a lay audience. Plus, as additional therapies for ocular surface healing emerge, our hope is that refractive surgeons can work alongside the ophthalmic community with patients to help stop STODS.
CONCLUSION
The RSA Terminology Committee hopes that the terms LR, LALEX, and STODS gain traction in the literature, achieve broad acceptance, and foster patient education, understanding, and communication.
Let’s Speak Lenspeak—Updated
Sheraz M. Daya, MD, FACP, FACS, FRCS(Ed), FRCOphth
Keeping up with IOL nomenclature is exhausting. The use of terms such as extended depth of focus (EDOF), enhanced monofocal, and even presbyopia-correcting can confuse both ophthalmologists and, more worrisomely, patients. It can also contribute to dissatisfaction when patients feel the IOL they received did not deliver the results they were expecting. This is unacceptable in the phenomenal age of advanced eye surgery. Consistent nomenclature could provide clarity to the stakeholders in the industry of vision restoration and correction—the providers (us), patients, and manufacturers. As an organization, the position of the American-European Congress of Ophthalmic Surgeons (AECOS) is that the use of clear, consistent language will enable providers and manufacturers to benefit from a bigger and more confident patient pool for premium lens surgery.
My article “Let’s Speak Lenspeak,” published in the February 2021 issue of CRST Europe, described the preliminary work undertaken by the AECOS Europe Working Group on Lens Terminology subcommittee.* (To read the article, click here.) The current article explains further refinements in terminology that we hope will be accepted universally.
BACKGROUND
Current IOL terminology often confuses range of focus (ROF), mechanism of action, and adverse effects like dysphotopsias. For example, the nomenclature EDOF IOL suggests that all lenses of this type behave similarly and can be used interchangeably. The criterion for an EDOF IOL—at least 50% of eyes achieving a monocular distance-corrected intermediate visual acuity of 0.2 logMAR (20/32) or better at 66 cm—was established by the American National Standards Institute (ANSI standard Z80.35-2018) and adopted by the AAO in 2015.1,2 AECOS believes 50% is too low, considering that we are prompting patients to make a choice based on trust that they will achieve reliable intermediate vision. Do the same odds as tossing a coin warrant counseling patients that they will have good quality intermediate vision?
There are myths and misconceptions surrounding EDOF lenses. Some clinicians tell patients that these IOLs are more forgiving, less likely to cause dysphotopsias, and easy to adapt to. Little consideration is paid to the ocular surface, corneal optics, lens positioning, axial length, and personality type during preoperative counseling. These issues are discussed in more detail in my previous article.
UPDATED TERMINOLOGY
Early recommendations. Overall, European ophthalmologists responded positively to and adopted the IOL terminology suggested by AECOS in 2021, which was to separate IOLs into two categories by ROF and mechanism of action. Some, however, insist that EDOF is a good term, even if it clouds the criteria for patient candidacy. AECOS then sought additional feedback from its membership and revised IOL nomenclature (Figure 1) and performance criteria (Figure 2) to be more inclusive of all lenses and, we hope, acceptable to both colleagues and patients.
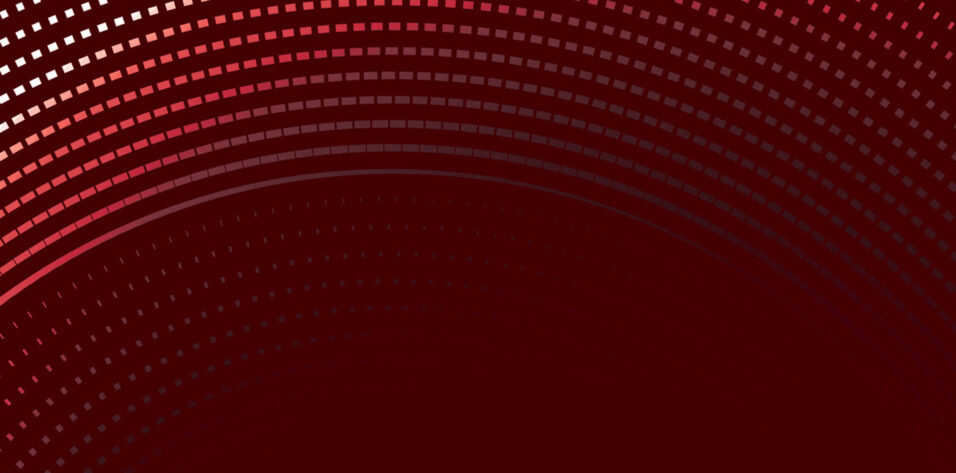
Figure 1. Updated IOL terminology (A), nomenclature (B), and mechanism of action (C) proposed by AECOS.
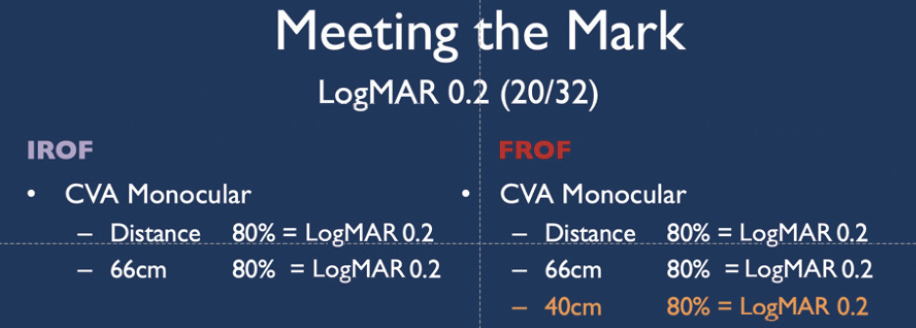
Figure 2. IROF and FROF IOLs.
Updated recommendations. IOLs are now categorized into three groups based on the components of ROF, mechanism of action, and dysphotopsias. This approach is akin to the gemological classification of diamonds into the 4 Cs (carat, color, clarity, and cut).
- Range of focus. ROF IOLs (Figure 1A) include monofocal (a fixed single-focus IOL), monofocal plus (a monofocal IOL that provides an increased ROF but does not meet the standard for an increased ROF IOL), increased ROF (IROF; achieves a monocular distance-corrected intermediate visual acuity of 0.2 logMAR [20/32] or better at 66 cm in 80% of eyes as opposed to 50% for EDOF IOLs), and full ROF (FROF; achieves 0.2 logMAR or better distance-corrected visual acuity, distance-corrected intermediate visual acuity at 66 cm, and distance-corrected near visual acuity at 40 cm simultaneously in at least 80% of eyes).
- Mechanism of action. The list has not changed since 2021 and may be found in Figure 1B. To some of us, a true EDOF IOL works by stretching the Circle of Least Confusion. Optical mechanisms such as a small aperture may achieve this elongation, and the mechanism is represented in the nomenclature. In Figure 1B, other is where future mechanisms can be included, and combined is for lenses with multiple optical mechanisms to achieve the same goal fit.
- Dysphotopsias. The AECOS Europe Working Group on Lens Terminology received no feedback on expanding the terms included in this group beyond glare, halos, and starbursts. It seems that patients do not use any other descriptions for dysphotopsias. We therefore did not add any terms but will revisit this in the future if regulatory authorities add snowballs and streaks to their list of dysphotopsia terms (Figure 3). Based on our review of manufacturer data, the incidence of dysphotopsias is low, and the effects decrease over time. Dysphotopsias become critical only when they are severe enough for patients to request IOL explantation. Of the more than 10,000 trifocal IOLs I have implanted in approximately 11 years, I have not explanted any for dysphotopsias (or any other reason). Our counseling and consent process is elaborate to ensure patients understand what to expect.
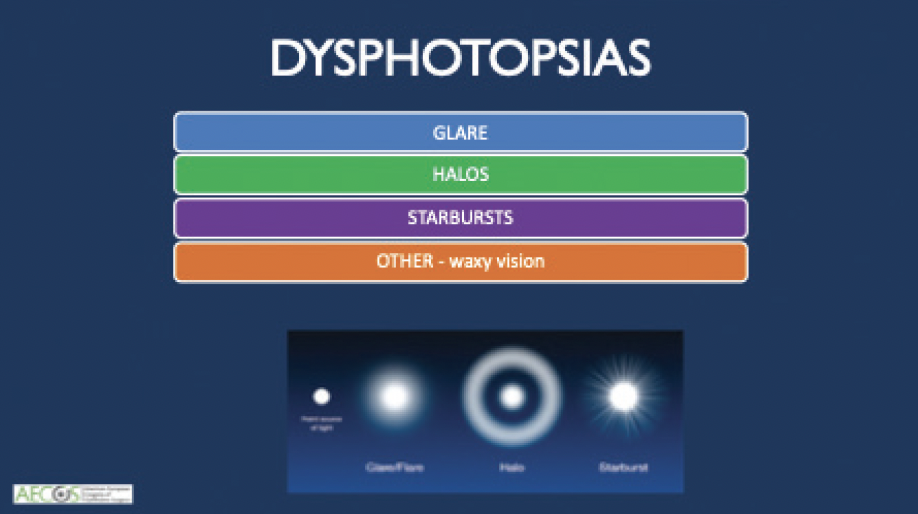
Figure 3. Terminology for dysphotopsias as recommended by AECOS.
AECOS encourages all surgeons to audit their personal data using the form found in Figure 4 (download the form by scanning the QR code). This can help ensure that IOLs meet the relevant criteria. It can also improve patient counseling about lens choices and relevant outcomes.
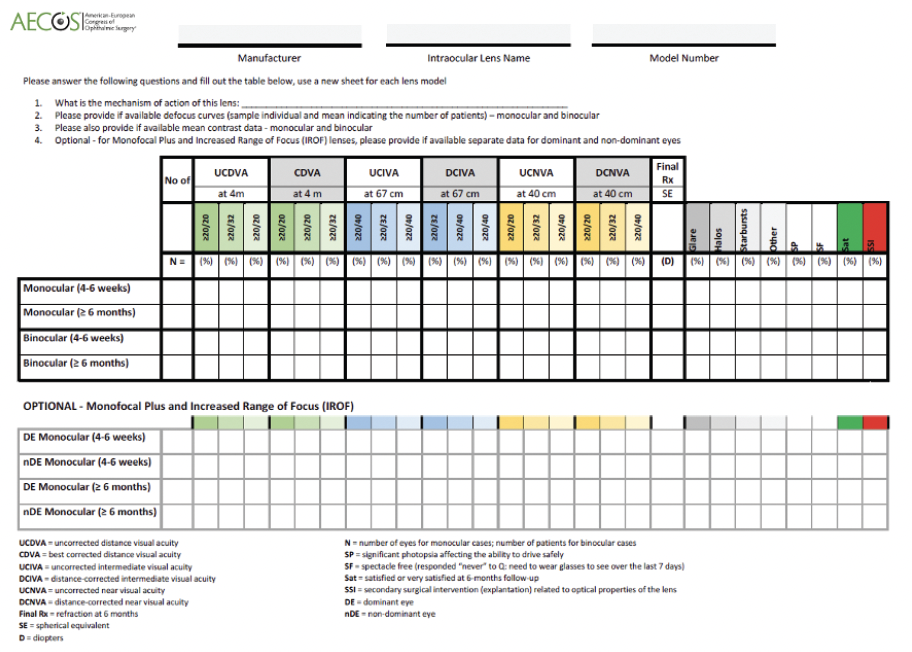
Figure 4. Personal data can be audited with this or a similar form.
CONCLUSION
IOL nomenclature should be simple and consistent and follow a uniform set of rules that can be adapted or expanded as needed. Most importantly, the nomenclature must be understandable to all stakeholders. AECOS is pleased that VSY, Hoya, and Voptica have already adopted the recommended IOL terminology. We hope that others will consider doing so because we believe it will improve both doctor and patient comprehension and satisfaction.
1. Draft consensus statement for comment. American Academy of Ophthalmology. October 7, 2015. Accessed January 22, 2021. Testing_for_EDOF_IOLs_Comment_Document_October_2015.pdf
2. MacRae S, Holladay JT, Glasser A, et al. Special report: American Academy of Ophthalmology task force consensus statement for extended depth of focus intraocular lenses. Ophthalmology. 2017;124:139-141.
*The authors wish to thank the other members of the RSA Terminology Committee and the RSA membership.
*AECOS Europe Working Group on Lens Terminology: Sheraz Daya, Erik Mertens, Francesco Carones, Joaquin Fernandez, and David Shahnazaryan