A significant percentage of the population experiences presbyopia.1 Phakic IOLs that correct presbyopia have emerged as an efficient remedy for patients seeking visual independence from glasses and contact lenses. To achieve successful outcomes, it is essential to optimize preoperative workflow.
AT A GLANCE
- Patient selection and education are key to success with presbyopia-correcting phakic IOLs.
- The choice of phakic IOL hinges on patients’ visual needs, ocular anatomy, and lifestyle factors.
- Efficient team coordination, precise surgical planning with advanced imaging technologies, and the management of preexisting ocular comorbidities are required to optimize surgical outcomes with presbyopia-correcting phakic IOLs.
PATIENT SELECTION AND EDUCATION
Success starts with patient selection and education. Choosing suitable candidates for presbyopia-correcting phakic IOLs requires conducting an extensive evaluation of their ocular health and refractive stability and, above all, setting realistic expectations. Patients should be educated on the advantages, potential risks, and limitations of the procedure. Clear communication is crucial to managing their expectations and promoting informed decision-making.
Understanding their lifestyle and visual needs is essential. An assessment of whether a patient participates in activities requiring superior distance, intermediate, or near vision can assist in defining the optimal depth of focus.
LENS CHOICE
The available lens designs and materials offer different degrees of near, intermediate, and distance vision correction. Understanding a patient’s visual needs, ocular anatomy, and lifestyle factors facilitates appropriate lens selection. Consideration of factors such as corneal endothelial cell density, anterior chamber depth (ACD), and iris anatomy can help reduce the risk of complications and guarantee long-term visual satisfaction. Currently, three presbyopia-correcting phakic IOLs are available.
ArtiPlus (Ophtec). This anterior chamber IOL has a multisegmented refractive aspheric optic that incorporates both far and near zones (Figure 1). It features a 6-mm optic in powers ranging from -15.00 to +2.00 D. Built on the Artisan phakic IOL platform (Ophtec), the ArtiPlus is constructed from polysiloxane. A 2.8-mm incision is required to implant the lens, and the ACD should be at least 2.8 mm from the corneal endothelium.

Figure 1. Rendering of the ArtiPlus iris-fixated phakic IOL for the correction of presbyopia.
Courtesy of Ophtec
An ongoing multicenter clinical study is evaluating the performance and safety of the ArtiPlus. The study enrolled adults with presbyopia requiring at least +1.00 D reading glasses and those predicted to have postoperative residual refractive cylinder of +1.00 D or less. Initial results are expected by year’s end.
Evo Viva ICL (STAAR Surgical). Also known as the Increased Range of Focus ICL (Figure 2), this IOL integrates advanced elements of the implantable collamer lens platform such as an increased optic diameter, the central port (KS-AquaPort), and an aspheric design, which theoretically extends depth of focus by about 2.00 D.2 It is made of collamer, a 100% pure collagen copolymer lens material, and has a dioptric range of -0.50 to -18.00 D.
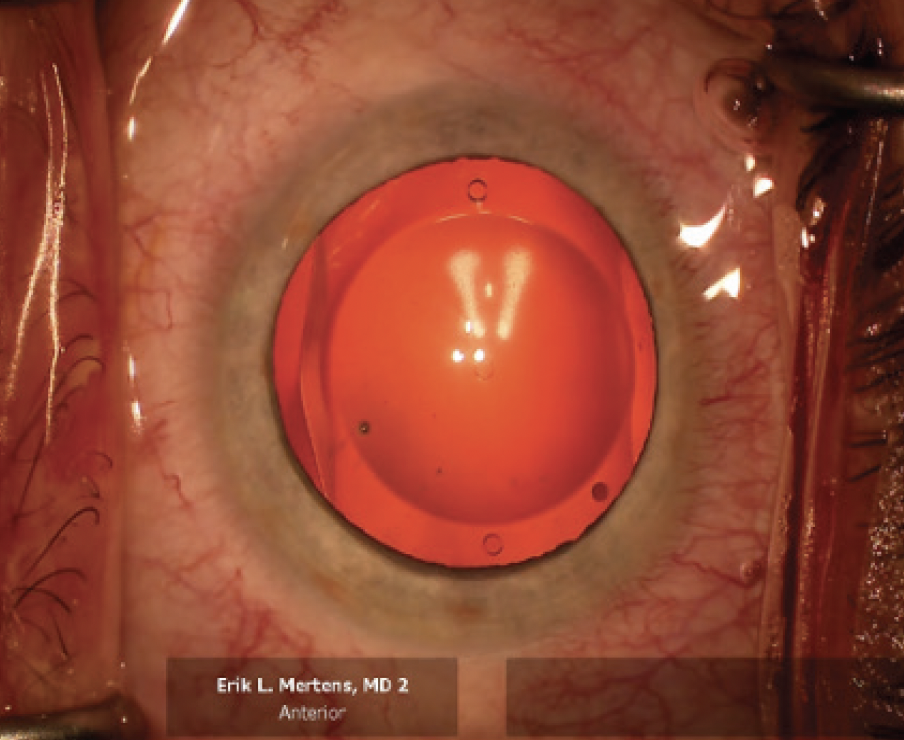
Figure 2. The Evo Viva ICL in vivo.
Courtesy of Erik L. Mertens, MD, FEBOphth
A 2.8-mm incision is required for lens implantation, and the ACD must be at least 2.8 mm. The IOL is suitable for patients aged 40 to 60 years who require an ICL power from -0.50 to -18.00 D, necessitating a reading addition of +1.00 to +2.50 D. They should have no more than 0.75 D of refractive astigmatism in either eye.
IPCL V2.0 Presbyopic (Care Group). This lens is available with a diffractive/refractive optic and is suitable for presbyopia correction in patients roughly 40 to 60 years of age who have not yet developed a cataract.3 The IPCL V2.0 Presbyopic is made of a hydrophilic hybrid acrylic material and is available in a dioptric range of -0.50 to -30.00 D for myopia and +0.50 to +6.00 D for hyperopia.4 The cylinder power range is +1.00 to +8.00 D with a customized cylinder axis. A 2.8-mm incision is required for IOL implantation, and the minimum ACD is 2.8 mm.
IPCLs have a central opening for unrestricted aqueous flow, eliminating the need for an iridectomy. The lens includes four additional holes in the periphery of the optic zone to facilitate aqueous flow. The IPCL has a diffractive optical zone of 5.8 mm and is available in near additions between +1.50 and +4.00 D. The optical diameter of the IPCL can be customized to accommodate large pupils, and the overall diameter of the IPCL ranges from 11 to 14 mm in 0.25-mm steps.
SURGICAL PLANNING AND SIMULATION
Precise surgical planning is required for successful outcomes. Following other practice tips outlined in the sidebar can also help promote positive outcomes with the procedure. Lastly, advanced imaging technologies such as anterior segment OCT (AS-OCT) and corneal topography and tomography can be instrumental for assessing corneal shape, anterior chamber dimensions, and angle anatomy. These tools aid in precise lens power calculations and iris claw sizing, thereby promoting optimal lens placement.
PRACTICAL TIPS
The following pointers can further improve preoperative workflow
- Establish a standard checklist to ensure all necessary preoperative evaluations, measurements, and assessments are complete
- Leverage educational materials such as brochures and multimedia presentations to enhance patient understanding and compliance
- Encourage patients to stop wearing contact lenses before preoperative measurements to improve the accuracy of ocular measurements and treat corneal irregularities such as epithelial thickness discrepancies, meibomian gland dysfunction, and/or low tear film breakup time
- Implement a tracking system to monitor and follow up with patients throughout the preoperative period
- Dedicate a staff member to addressing patient queries and concerns
Simulation software and IOL calculation formulas such as the LASSO family further refine surgical planning, enabling surgeons to envision potential outcomes and adjust parameters preoperatively.5
TEAM PREPARATION AND SCHEDULING
Efficient coordination and preparation of the team help streamline preoperative workflow. Establishing clear protocols for patient evaluation, diagnostic testing, and consultations can expedite the process. Communication between the surgeon, optometrists, nurses, and support staff should be clear to promote the timely sharing and application of critical information. The use of an electronic medical record system and integrated scheduling software can boost efficiency, reduce errors, and improve patient flow.

Figure 3. The IPCL V2.0 Presbyopic lens.
Courtesy of Care Group
COMORBIDITY MANAGEMENT
Conditions such as dry eye disease, corneal irregularities, and mild cataract may affect the choice of phakic IOLs or necessitate additional preoperative treatment. Addressing dry eye disease before surgery can enhance ocular surface health, improve visual quality, and reduce the risk of postoperative complications. Collaborating with cornea, glaucoma, and retina specialists can facilitate comprehensive comorbidity management.
1. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia. Ophthalmology. 2018;125(10):1492-1499.
2. Packer M, Alfonso J, Aramberri J, Elies D, Fernandez J, Mertens E. Performance and safety of the extended depth of focus implantable collamer lens (EDOF ICL) in phakic subjects with presbyopia. Clin Ophthalmol. 2020;14:2717-2730.
3.Stodulka P, Slovak M, Sramka M, Polisensky J, Liska K. Posterior chamber phakic intraocular lens for the correction of presbyopia in highly myopic patients. J Cataract Refract Surg. 2020;46(1):40-44.
4. Schmid R, Luedtke H. A novel concept of correcting presbyopia: first clinical results with a phakic diffractive intraocular lens. Clin Ophthalmol. 2020;14:2011-2019.
5. Rocamora L, Orlando JI, Lwowski C, Kohnen T, Mertens E, Van Keer K. Postoperative vault prediction for phakic implantable collamer lens surgery: the LASSO formulas. J Cataract Refract Surg. 2023;49(2):126-132.