During the past year in our practice, we have begun performing early refractive lens exchange (RLE) surgery in selected patients in their 40s—well before the age when one typically considers lens-based surgery. But today, every refractive surgeon faces this conundrum on a regular basis when Generation X patients—those in their late 30s or their 40s—come in for refractive surgery consultations. Maybe they are interested in LASIK; maybe they saw a commercial on TV for corneal inlays. These patients are at a point in their lives at which they have the stability, time, and financial means to finally do something about wearing glasses.
But we know that, at age 45, they are already presbyopic, and their symptoms are likely increasing. Laser vision correction won’t help them see at near unless a monovision procedure is considered. Corneal inlays could be an excellent solution, except that many of these patients are far from emmetropic and would also require LASIK to take advantage of the inlay’s effect. High ametropes may not even be good candidates for LASIK due to thin corneas and risk of ectasia from the amount of tissue that would have to be ablated for the required correction.
So, what procedure would best benefit these patients?
Recently, I have begun to think that lens-based surgery may actually represent the best option for presbyopic high myopes or hyperopes with astigmatism. For the first time, we now have IOLs that can correct all their refractive errors and address presbyopia at the same time. Although it means giving up their remaining natural accommodation, lens surgery might be the only way to achieve the goal of spectacle independence without multiple procedures. My patients who have opted for early lens surgery also like the fact that they won’t have to worry about a complicated postrefractive surgery IOL power calculation or cataract surgery in the future.
IMPROVEMENTS IN TECHNOLOGIES
New surgical technologies have made it possible to broach the conversation with patients about early lenticular surgery. The most important change, from my viewpoint, has been the advent of premium multifocal and extended depth of focus (EDOF) IOLs that can also correct astigmatism. Previously, our parameters for treatment were much narrower: If we could not reliably correct astigmatism when implanting a multifocal IOL, we could not really satisfy the astigmatic patient whose goal was to get rid of glasses. In the United States today, we have lenses like the AcrySof IQ ReStor Multifocal Toric (Alcon), the Tecnis Symfony EDOF Toric (Johnson & Johnson Vision), and the Trulign Toric (Baush + Lomb); in Europe, even more toric lenses are available to astigmatic patients.
The availability of laser cataract surgery has also opened avenues for patients with astigmatism in addition to high refractive error. We can now use the laser to create arcuate incisions to correct up to 1.00 or 1.50 D of astigmatism. The laser also facilitates a two-point chop and creates a perfect capsulorrhexis for optimal lens centration and stability. Finally, we cannot discount the role of other pre- and intraoperative technologies that aid in the process of providing these young patients with the best possible outcomes. For me, these include the ORA System with VerifEye+ intraoperative aberrometer (Alcon); the Cassini topographer (iOptics), which can reliably measure posterior corneal curvature; and improved IOL power calculation methods such as the Hill RBF formula and the Barrett toric calculator.
None of these technologies is a guarantee of a perfect outcome. Taken together, however, they significantly increase my confidence in predicting visual outcomes with accuracy and precision.
VALUE PROPOSITION
Because these younger patients do not yet have cataracts, a lens procedure won’t be even partially covered by insurance. At approximately double the cost of LASIK, there is no question that the price tag of RLE with a premium IOL is a barrier for many patients. But several recent experiences have encouraged me to think differently about price versus value.
We probably all counsel our 60-, 70-, and even 80-year-old patients that premium lenses can provide a once-in-a-lifetime opportunity for spectacle independence. After their surgeries, many of these patients say to me, “Wow, I didn’t know what I was missing. I wish I’d had this done earlier!” On the flip side, I have had 85-year-old cataract patients make the calculation that the additional cost of a premium lens isn’t worth it because they feel that their expected remaining life span is short.
This got me thinking about the tradeoffs and about what our patients value. They know they are eventually going to have intraocular surgery. If given a choice, many might prefer to undergo the risks of intraocular surgery earlier in life in order to enjoy the benefits of enhanced vision over a longer period.
INFORMED CONSENT
It is imperative to have a thorough informed consent process. To me, there are two main issues that require honest and transparent discussion.
No. 1: The assumption of risk. Every surgery has risks, however small. These young patients are assuming the risks of intraocular surgery—infection, inflammation, retinal detachment, or a surgical complication—20 years or more before they need cataract surgery. I explain the risks of surgery, but I also share with patients how much surgery we do and how safe and effective lens procedures are in our hands. Our rate of all serious risks combined is less than 3%, and our rate of endophthalmitis is well below 1% (personal data). I tell them that we have invested in a lot of technologies to make our results as safe and effective as possible.
No. 2: The potential for future ocular conditions to develop. Young RLE patients have many years ahead in which they could develop glaucoma, macular degeneration, or some other condition that might make having a presbyopia-correcting IOL less desirable. In order to be reasonably confident that the lens will meet the patient’s needs for the rest of his or her lifetime, we must elicit a careful family history and perform a thorough battery of diagnostic tests including pachymetry and OCT of the macula, retinal nerve fiber layer, and ganglion cell complex to identify any risks (Figure). While one must have an honest discussion about this topic with patients, I believe the probability of serious future concerns is quite low in heathy eyes, particularly in light of the benefits of premium lens surgery to be enjoyed.
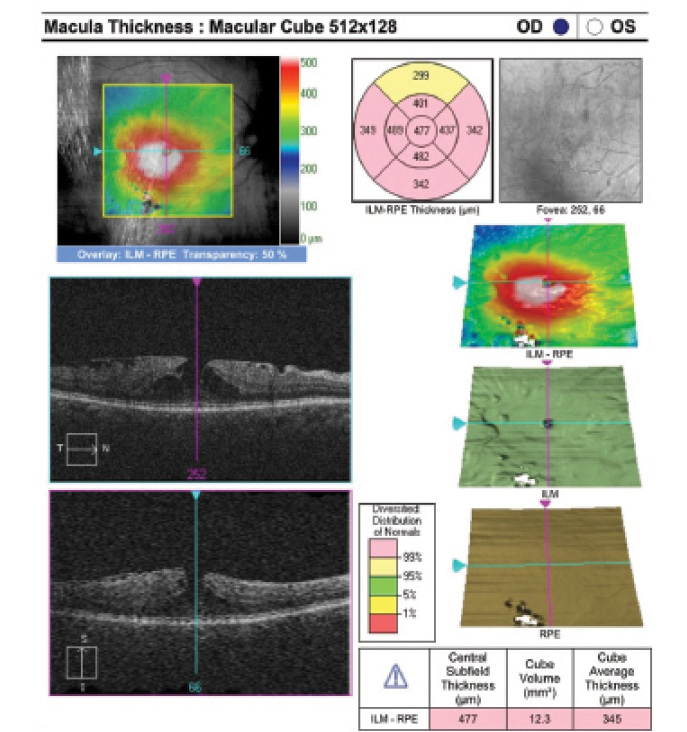
Figure. Preoperative macular OCT shows that this patient is not a good candidate for an EDOF or multifocal IOL due to the presence of an epiretinal membrane with a lamellar macular pseudohole.
CONCLUSION
Early RLE is not something I undertake every day. Increasingly, however, I consider it as a serious option for patients in their 40s who have high refractive errors and who desire spectacle independence.