CASE PRESENTATION
A 21-year-old woman underwent bilateral CXL for mild keratoconus (Figure 1). Four years later, an examination revealed significant improvement in corneal shape and BCVA (to 20/25) in both eyes. The patient has mild myopia with astigmatism in both eyes. Her corneas are clear with no haze (Figure 2).
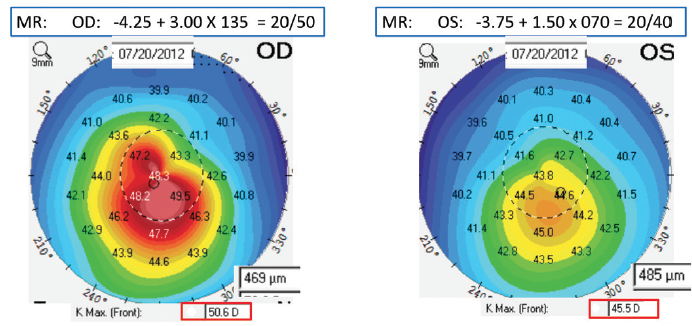
Figure 1. The patient had mild keratoconus, more significant in her right than left eye.
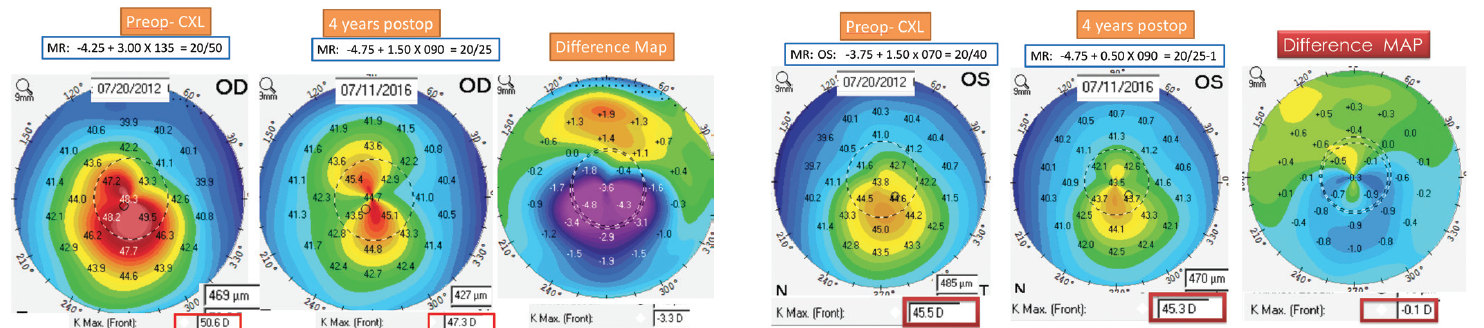
Figure 2. At 21 years of age, the patient underwent bilateral CXL in August 2012. Four years postoperative, the patient expressed a desire to reduce her need for contact lenses or glasses.
The patient is an outdoors person, and she enjoys activities for which contact lens wear can be challenging such as kite surfing. She would like to explore the possibility of undergoing refractive surgery to improve her UCVA. How would you proceed?
—Case prepared by William B. Trattler, MD

PARAG A. MAJMUDAR, MD
We refractive surgeons will be seeing many more cases like this one as greater numbers of patients with mild to moderate keratoconus undergo CXL and as our thinking about the treatment of keratoconus shifts. CXL has already allowed us to change from reactive to proactive mode; no longer do we wait for corneal transplantation. I believe that topography-guided excimer laser ablation heralds the next phase of keratoconus treatment: improving the shape of the cornea and reducing patients’ sometimes crippling dependence on rigid or scleral contact lenses.
This patient’s corneas have experienced significant flattening and remodeling since undergoing CXL. Additionally, the keratoconic process appears to have stabilized, and her BCVA has improved. In my opinion, topography-guided PRK would be the best option for reducing her dependence on corrective lenses.
Patients with keratoconus are often married to their contact lenses, and that dependence can become burdensome as they age and experience increased ocular surface dysfunction. For that reason, many of them hope for a procedure that will allow them to wear spectacles—an option that individuals without the disease generally take for granted. We surgeons must explain to keratoconic patients seeking refractive correction that corrective surgery may not improve their visual acuity to 20/20 and eliminate their need for glasses or contact lenses; instead, we are trying to reduce their higher-order corneal aberrations so that they can wear spectacles or daily disposable soft contact lenses.
I would offer this patient topography-guided ablation, one eye at a time. I would instruct her to discontinue contact lens wear 2 weeks prior to the evaluation in order to achieve the most accurate preoperative readings. I would aim to correct the majority of the topography-derived refraction rather than the manifest refraction, and I would limit the ablation to approximately 50 µm. In the event that full correction called for more than 50 µm of ablation, I would advise the patient that she might have residual refractive error. In certain cases, more complete refractive correction can be attained, but it is important to set the patient’s expectations appropriately. Many times, topography-guided ablations induce myopia or hyperopia; if they are not compensated for in the original treatment, a second procedure may be necessary, and patients should be forewarned of that possibility. I believe that, in the future, we may be able to combine CXL and topography-guided PRK as a primary procedure.
An area that requires further investigation in cases such as this one, where CXL was performed at an earlier date, is whether or not repeat CXL should be performed at the time of topography-guided PRK. As greater numbers of patients are treated and these concepts are explored further, I look forward to being able not only to arrest the progression of keratoconus but also to rehabilitate these patients and reduce their dependence on contact lenses.

RICCARDO VINCIGUERRA, MD
A keratoconic patient with good or excellent BCVA after CXL who wants to improve her UCVA is an interesting case.
I would not consider any surgery that entailed weakening the cornea, such as PRK, LASIK, or small-incision lenticule extraction. I always give the example of the leaning tower of Pisa: If it is stable, you do not want to push it! For this reason, I would consider either the Visian ICL (STAAR Surgical) or no surgery at all.
If the patient satisfies the criteria for an ICL (ie, anterior chamber depth, no cataract or glaucoma), I would look at three main things. First, is the flattening effect produced by CXL stable? If the cornea is still changing, implanting an ICL would not be wise. Second, is the corneal astigmatism regular and significant? Third, is the spherical refractive error significant? If so, as in the patient’s right eye, I would implant a Visian Toric ICL (TICL) because it should provide excellent visual acuity without weakening the cornea. If the astigmatism is regular but not high and the spherical refractive error is significant, as in the patient’s left eye, then I would implant the Visian ICL rather than the toric model. If the astigmatism is irregular and high and the spherical refractive error is significant, I would also implant the Visian ICL rather than the Visian TICL because the latter would not correct the coma induced by keratoconus and would leave the patient unsatisfied. If the patient had irregular astigmatism and no significant spherical refractive error, I would not suggest any surgery.
Prior to any surgical intervention, thorough informed consent would be mandatory to explain to the patient that the procedure will achieve only a partial correction.

WHAT I DID: WILLIAM B. TRATTLER, MD
The patient achieved a significant improvement in corneal shape and quality of vision after her CXL procedure in 2012. We discussed the various treatment options with the potential to reduce her need for contact lenses or glasses, including Intacs (Addition Technology) and PRK. Because the Visian TICL is not available in the United States, it was not an option for this patient. She felt most comfortable with PRK.
The patient and I discussed her situation in detail. I thoroughly explained that her corneas were stronger and less irregular since her CXL procedure, leading to her improved BCVA. I also emphasized that her corneas were on the thin side, however, and I made her aware that undergoing PRK carried a risk of recurrent keratoconus. With the understanding that she would need to return to the office annually for corneal mapping, the patient opted to move forward with bilateral PRK with mitomycin C 0.02% for 12 seconds in autumn 2016.
One year postoperatively, the patient reported that she was pleased with her UCVA. Her corneal shape had improved significantly in both eyes, with no signs of keratoconus recurrence. She was instructed on the importance of avoiding eye rubbing and will return this autumn for repeat corneal mapping with the Pentacam (Oculus Optikgeräte).