The popularity of phakic IOLs has rapidly increased in recent years. Although both laser vision correction and lens-based refractive surgery can help patients achieve 20/20 vision without the need for glasses or contact lenses, these are two very different procedures. In the field of refractive surgery, LASIK has in many ways captured the attention of the public, but phakic IOLs also have a lot to offer for appropriately selected patients.
I started implanting anterior chamber phakic IOLs in 1992, and I switched to posterior chamber phakic IOLs in 2003. Over the years since I started, the importance of this procedure has only grown in my practice. The reasons for this are plentiful, and I describe some here.
AT A GLANCE
- Phakic IOLs are intended to be permanent, but, if results are unsatisfactory, they can be removed, allowing the eye to return to its original condition.
- Other advantages of phakic IOLs over cornea-based refractive surgery approaches include predictability, fewer DED problems after surgery, and improvements in quality of vision.
- Phakic IOLs have evolved from a niche product into a mainstream surgical option. Dr. Mertens predicts that their popularity will continue to grow exponentially in the near future.
WHY IT GROWS
Reversibility. First, phakic IOLs are intended to be permanent, but, if results are unsatisfactory, they can be removed, allowing the eye to return to its original condition. This reversibility, in contrast with the permanence of corneal ablation in laser vision correction, is a very important factor. I have had many patients express their willingness to undergo phakic IOL implantation, even though it requires an incision in the eye, because it does not induce permanent change the way that corneal refractive surgery does.
When we change the curvature of the cornea, future options are greatly reduced. As has been pointed out in the literature,1,2 corneal refractive surgery patients are almost 2.5 times more likely to have worse postoperative distance BCVA after cataract surgery than nonrefractive surgery patients. This difference is because of two reasons: induced higher-order aberrations in the cornea and reduced accuracy of IOL calculations in these patients.
Predictability. Another important reason why surgeons and patients opt for phakic IOLs is their predictability and stability. The Figure on the following page shows my personal results in 306 eyes. The coefficient of determination (R2) of 0.9992 in this series confirms the reliability of the postoperative results. By contrast, Lim et al found that moderately myopic eyes showed progressive myopic shift and corneal thickening after LASIK and LASEK during 10 years of follow-up.3 Those authors concluded that early refractive regression may indicate long-term refractive outcome.
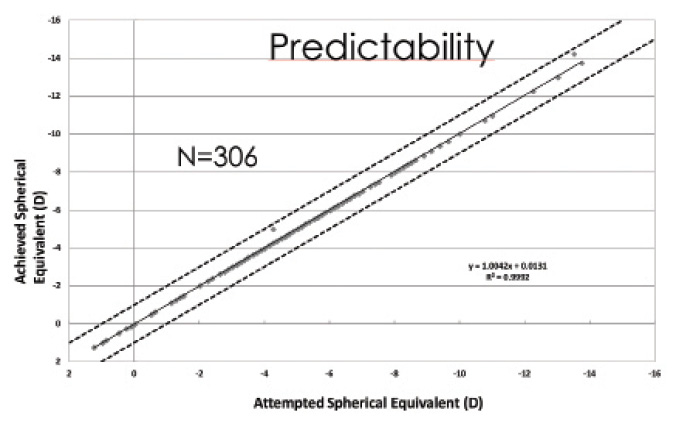
Figure. Predictability of the Visian ICL in 306 eyes.
Dry eye issues. The topic of dry eye disease (DED) in relation to refractive surgery is subject to much debate. There is nothing more frustrating for the surgeon than dealing with a patient who is unhappy postoperatively because of DED issues.4,5 Preoperative screening and counseling are of utmost importance in detecting and ameliorating DED before surgery. I started looking into this 6 years ago in patients who consulted me to undergo refractive surgery and found that a high percentage of these patients could potentially have had DED problems if corneal surgery had been pursued. Patient satisfaction at 1 month after surgery went up significantly with phakic IOL implantation, minimizing DED problems after refractive surgery.
Quality of vision. Finally, quality of vision is an important reason that many patients favor phakic IOLs over corneal refractive surgery. As we deal most of the time with young myopes with large pupils in our daily lives as refractive surgeons, we must carefully consider which procedure will provide them with excellent night vision and overall satisfaction with their visual quality. One recent study concluded that low-luminance visual acuity and contrast sensitivity significantly improved in patients after implantation of the Visian ICL (STAAR Surgical), and these improvements were significantly greater than those observed after wavefront-optimized LASIK.6 These findings support those of the US FDA trial of the ICL, which demonstrated improved night vision performance following ICL implantation.7
CONCLUSION
After carefully considering these strong points in favor of phakic IOLs, surgeons should always decide which procedure to choose in the best interests of the patient. Phakic IOLs have evolved from a niche product into a mainstream surgical option, the popularity of which I believe will continue to grow exponentially in the near future.
1. Schuster AK, Schanzlin DJ, Thomas KE, et al. Intraocular lens calculation adjustment after laser refractive surgery using Scheimpflug imaging. J Cataract Refract Surg. 2016;42(2):226-231.
2. Manning S, Barry P, Henry Y, et al. Cataract surgery outcomes in corneal refractive surgery eyes: Study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg. 2015;41(11):2358-2365.
3. Lim SA, Park Y, Cheong YJ, Na KS, Joo CK. Factors affecting long-term myopic regression after laser in situ keratomileusis and laser-assisted subepithelial keratectomy for moderate myopia. Korean J Ophthalmol. 2016;30(2):92-100.
4. Xie W. Recent advances in laser in situ keratomileusis-associated dry eye. Clin Exp Optom. 2016;99(2):107-112.
5. Chao C, Golebiowski B, Zhao X, et al. Long-term effects of LASIK on corneal innervation and tear neuropeptides and the associations with dry eye. J Refract Surg. 2016;32(8):518-524.
6. Parkhurst GD. A prospective comparison of phakic collamer lenses and wavefront-optimized laser-assisted in situ keratomileusis for correction of myopia. Clin Ophthalmol. 2016;10:1209-1215.
7. Sanders DR, Doney K, Poco M, for the ICL in Treatment of Myopia Study Group. United States Food and Drug Administration clinical trial of the Implantable Collamer Lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111(9):1683-1692.



