Laser corneal refractive surgery precisely changes corneal curvature to compensate for refractive errors of the eye. Although the refractive outcomes of SMILE are not influenced by intraoperative dehydration of the cornea, as they are in LASIK, other factors can affect postoperative outcomes. These factors may be categorized as extrinsic (ie, patient-based, preoperative) and intrinsic (ie, inherent to the method itself, laser-based, intraoperative). My colleagues and I conducted three studies to identify as many of these factors as possible.
STUDY NO. 1
Methodology. This retrospective chart review was conducted across three centers.1 It involved a total of 2,564 eyes of 1,524 consecutive patients undergoing SMILE for the correction of myopia or myopic astigmatism between 2015 and 2019. All eyes had normal keratometry and topography, and retreatments were not considered.
All analyses were run four times, once for each dataset and once with the global dataset. We evaluated whether some parameters affected all three clinics and were thus likely to be inherent to the procedure and whether some parameters affected only one dataset and were thus likely depending on the surgeon or clinic.
Results. At all three centers, percentagewise, refractive outcomes were most accurate overall for high corrections. On average, attempted corrections of -1.00 and -13.00 D resulted in undercorrections of -0.14 and -0.80 D, respectively (Table 1).
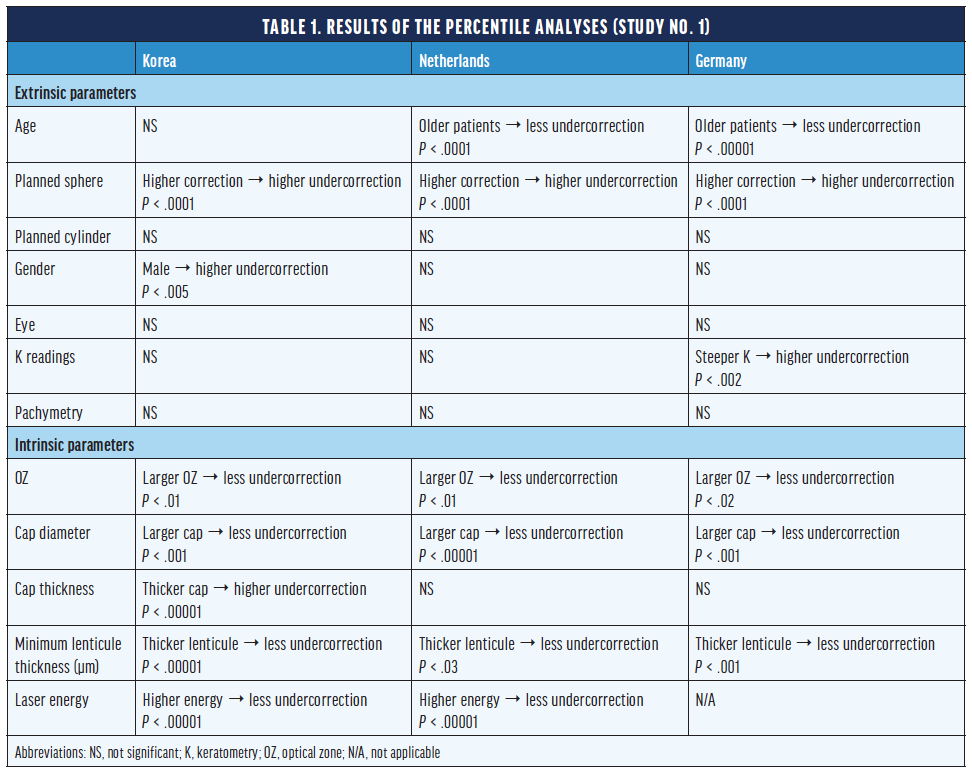
Higher corrections and older patients showed relative undercorrections of almost 1% per diopter of planned correction or per decade of age. Female patients showed relative overcorrections (> 1%) compared with male patients. There was a systematic undercorrection (-0.40 D). Other parameters did not show statistical significance at all three practices.
Discussion. In our global trends analysis, age and planned sphere were the only extrinsic parameters that had a consistent impact on outcomes. Among intrinsic parameters, only cap thickness did not show a systematic effect (range, 100–140 µm). The optical zone diameter, cap diameter, and minimum lenticule thickness consistently affected refractive outcomes at all three centers.
Seasonal variations in postoperative outcomes were found. Treatments performed in the spring produced relative overcorrections of the spherical equivalent, whereas procedures performed in the summer produced relative undercorrections of the spherical equivalent (both P < .05).
STUDY NO. 2
Methodology. This prospective multicenter case series assessed whether flushing the interface with balanced saline solution during SMILE affected refractive outcomes.2
All patients (n = 470 eyes) had myopia or myopic astigmatism of similar magnitude in both eyes, a spherical equivalent of 10.00 D or less, preoperative corrected distance visual acuity of 0.80 or better, and anisometropia of 2.00 D or less. All patients underwent bilateral SMILE. The interface of only one eye of each patient was flushed after dry extraction of the lenticule.
Results. One day after surgery, mean uncorrected distance visual acuity was 0.81 in the unflushed eyes and 0.83 in the flushed eyes (P = .110). Three months after surgery, mean uncorrected distance visual acuity was 1.04 in the unflushed and 1.05 in the flushed eyes (P = .172). No significant difference in the rate of postoperative complications was found.
Discussion. Flushing the interface during SMILE presented no advantages or disadvantages in terms of visual recovery, postoperative complications, or final visual acuity.
STUDY NO. 3
Methodology. The purpose of this study was to evaluate how a thin cap affects the following with SMILE for the correction of myopia or myopic astigmatism: postoperative spherical equivalent refraction, cylinder, BCVA and UCVA, and ease of lenticule separation.3 The charts of 51 patients (102 eyes) were reviewed, and the effects of caps that were 120 and 100 µm thick were assessed in a contralateral manner; all other laser parameters were kept constant.
Results. Visual acuity was similar in both groups as early as 1 day after surgery (Table 2). Three months after surgery, the spherical equivalent refraction was undercorrected in the 120-µm group relative to the 100-µm group, but the difference was not statistically significant. Postoperative cylinder was not statistically different between the two groups, and visual acuity was similar in both groups.
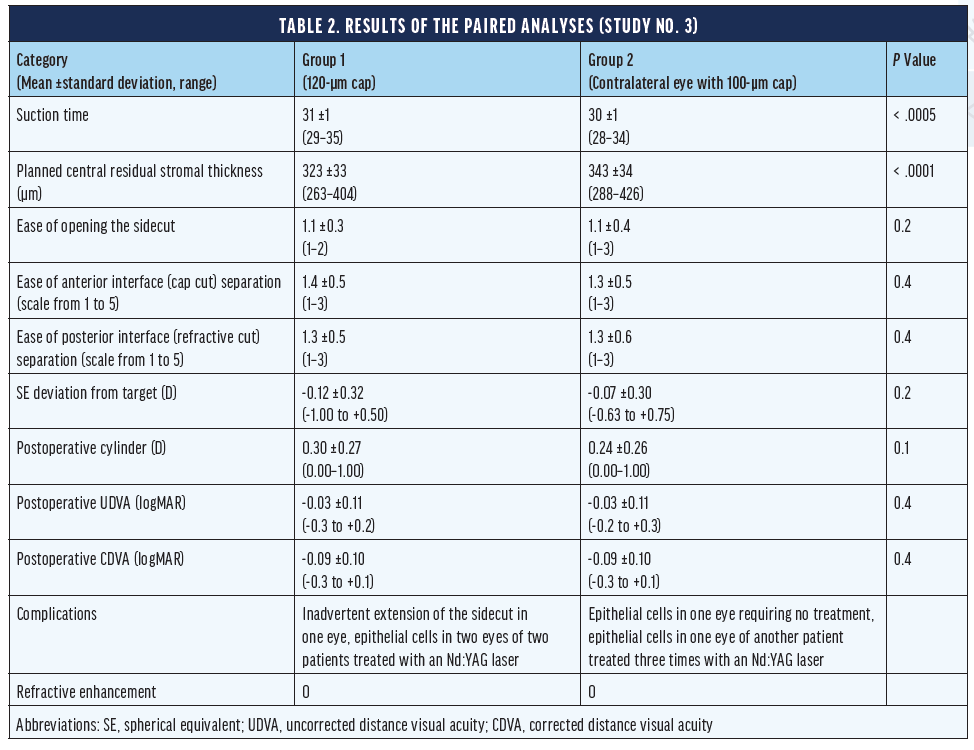
Ease of lenticule separation was identical in both groups. Postoperative central residual stromal thickness was 20 ±15 µm thicker with a 100-µm cap (P < .0001) as expected. The incidence of adverse events was comparable in the two groups.
Discussion. Cap thickness did not significantly affect postoperative refraction, visual acuity, the ease of lenticule separation, or the incidence of adverse events. Based on these results, surgeons can safely use a 100-µm cap without adjusting their nomograms when modifying from a standard thickness of 120 µm. If suction is lost during the lenticule cut of a 120-µm cap, a second docking with a programmed cap thickness of 100 µm (and a larger optical zone) may permit surgeons to perform the intended SMILE procedure, thus reducing the severity of this dreaded complication.
1. Arba-Mosquera S, Kang DYS, Luger MHA, Taneri S. Influence of extrinsic and intrinsic parameters on myopic correction in small incision lenticule extraction. J Refract Surg. 2019;35(11):712-720.
2. Kind R, Kiraly L, Taneri S, Troeber L, Wiltfang R, Bechmann M. Flushing versus not flushing the interface during small-incision lenticule extraction. J Cataract Refract Surg. 2019;45(5):562–568.
3. Taneri S, Arba-Mosquera S, Rost A, Hansson C, Dick HB. Results of thin-cap small-incision lenticule extraction. J Cataract Refract Surg. November 2, 2020. doi:10.1097/j.jcrs.0000000000000470